Systemic sclerosis, also known as scleroderma, is a rare disease characterized by the thickening and scarring of connective tissue of multiple organs in the body. The scarring can also affect the lungs and when this occurs the condition is called systemic sclerosis with interstitial lung disease, or SSc-ILD.
It is estimated that systemic sclerosis with ILD affects up to 86,000 people in the United States and 200,000 people in Europe, making it an orphan, or rare disease.
The disease impacts four times as many women as men, and the onset of the disease typically occurs at a young age – between 25 and 55 years, when they are deeply engaged in building careers and caring for family.
What are the main symptoms?
It is difficult to diagnose systemic sclerosis because its symptoms are similar to other autoimmune diseases. The first symptoms in most patients include Raynaud phenomenon (color changes of the fingers, typically induced by cold) and acid-reflux (GERD).
Nearly all people with systemic sclerosis have thickening of the skin, which can lead to contractures, ulcers and pain.
Shortness of breath is a common symptom caused by ILD and/or pulmonary hypertension. Other common symptoms of systemic sclerosis include arthritis and muscle weakness.
Which organs in the body does systemic sclerosis affect?
Skin thickening is the defining feature of scleroderma; internal involvement is the reason this disease is called “systemic sclerosis”.
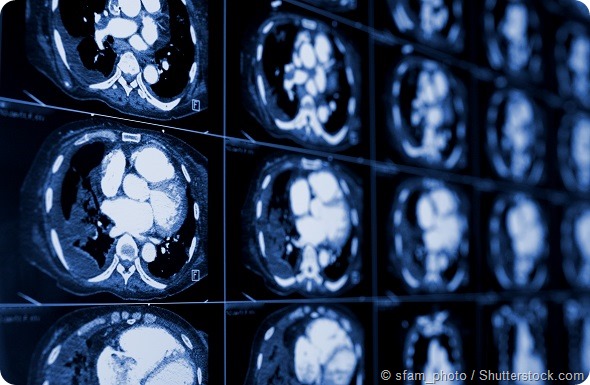
ILD is the result of inflammation and scarring in the lungs, and is one of the leading causes of death among people with systemic sclerosis. Gastrointestinal, heart and kidney involvement can also lead to substantial morbidity and mortality.
Why does the presence of interstitial lung disease (ILD) with systemic sclerosis often indicate a poor prognosis and higher risk of death?
The presence of inflammation and scarring (fibrosis) in the lungs can result in an accelerated and progressive decline in lung function. As lung function declines, patients become more easily short of breath and generally require more and more supplemental oxygen in order to maintain normal oxygen levels in the blood.
If blood oxygen levels cannot be maintained, death ensues. Currently, there are no approved treatments to halt or reverse the progression of scleroderma related ILD, and few drugs have been assessed in clinical trials for this disease.
How does systemic sclerosis with interstitial lung disease impact people’s lives?
Scleroderma related ILD results in progressive shortness of breath and cough. Patients may need supplemental oxygen. This leads to increasing difficulty with maintaining a job, performing daily activities and maintaining independence. This can have a substantial impact on a patient’s quality of life and may lead to anxiety and depression.
What research is needed into scleroderma?
There are no approved treatments for scleroderma or systemic sclerosis-ILD, which is a leading cause of morbidity and mortality in SSc. Research is key to help people living with scleroderma as few drugs have shown any efficacy in clinical trials for systemic sclerosis or SSc-ILD.
The SENSCIS™ (Safety and Efficacy of Nintedanib in Systemic SClerosIS) study is an important step in addressing this unmet need. The trial will help to further inform the medical community about this disease and whether a drug called nintedanib could be an effective therapy.
How much do you think can be learned from other rare lung diseases that cause scarring, such as idiopathic pulmonary fibrosis (IPF)?
Research in another rare lung disease called idiopathic pulmonary fibrosis, or IPF, provided important insights in how lung scarring develops and progresses, and led to the development of the first treatments for the disease.
One of these treatments, known as nintedanib, which is marketed as OFEV®, has been shown to slow disease progression as measured by annual rate of decline in lung function.
Because systemic sclerosi -ILD and IPF share similarities in how the underlying lung scarring or fibrosis, forms in people with the disease, the SENSCIS™ study will evaluate the impact of nintedanib on lung fibrosis associated with systemic sclerosis.
What do you think the future holds for systemic sclerosis patients?
The SENSCIS™ trial will help to further inform the medical community about systemic sclerosis -ILD and whether nintedanib could be an effective therapy.
People living with this disease are in need of treatment options, so this study is an important step in helping those patients and their families.
Where can readers find more information?
For more information, please visit clinicaltrials.gov/ct2/show/NCT02597933.
About Dr Kristin Highland
Dr. Highland is fellowship-trained in both pulmonary/critical care and rheumatology. She is a member of the Respiratory Institute of the Cleveland Clinic Foundation located in Ohio.
Her clinical practice is composed of complex patients with interstitial lung disease, pulmonary hypertension, sarcoidosis, and the pulmonary complications of the rheumatic diseases, including scleroderma.
Dr. Highland’s research interests have focused on interstitial lung disease and pulmonary hypertension with an emphasis on scleroderma.