The most recent complete data for England (2014/15) shows an average uptake of the guaiac Faecal Occult Blood Tests (gFOBT) from those invited by the NHS Bowel Cancer Screening Programme (BCSP) of 58.22%.
The average uptake is contributed to by a group of ‘convinced’ participants whose average uptake is typically 86% and this hides an uptake of 12% amongst a large ‘reluctant’ group who consistently choose not to participate.
This ‘reluctant’ group comes from the whole of England but is particularly in evidence in cities and amongst deprived populations. Sadly groups with the highest risk of bowel cancer have the lowest participation rate!
What does the new test involve and how does it differ from the current guaiac Faecal Occult Blood Test (gFOBT)?
The new test is called ‘FIT’ which is short for the Faecal Immunochemical Test for hemoglobin. It was developed in the 1990’s and was shown to be markedly better in detecting bowel cancer than any other simple screening test including that currently used by the UK program. It was recommended in 2010 for use throughout Europe and was first proposed for use in the NHS in 2009.
Screening
The test can measure the amount of human blood in stool and can do so at very low concentrations which enables detection of blood released from early cancers and polyps which might develop into cancers.
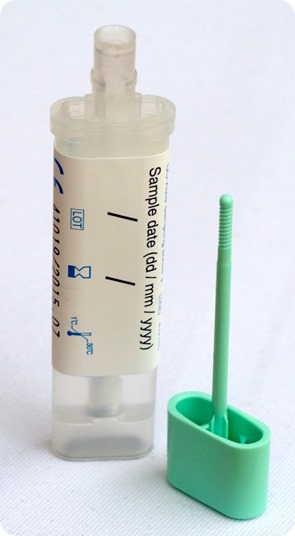
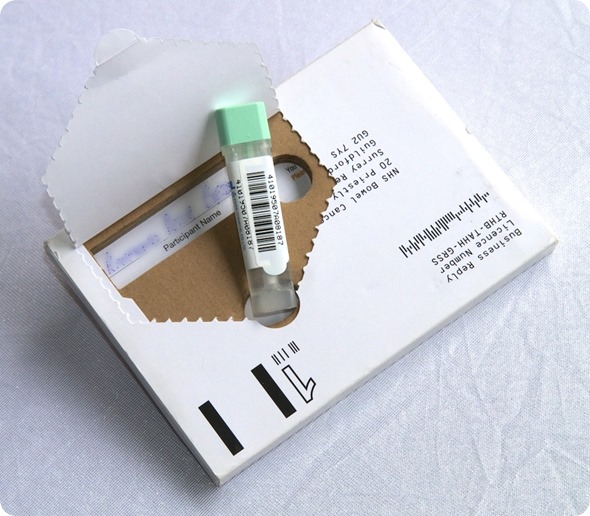
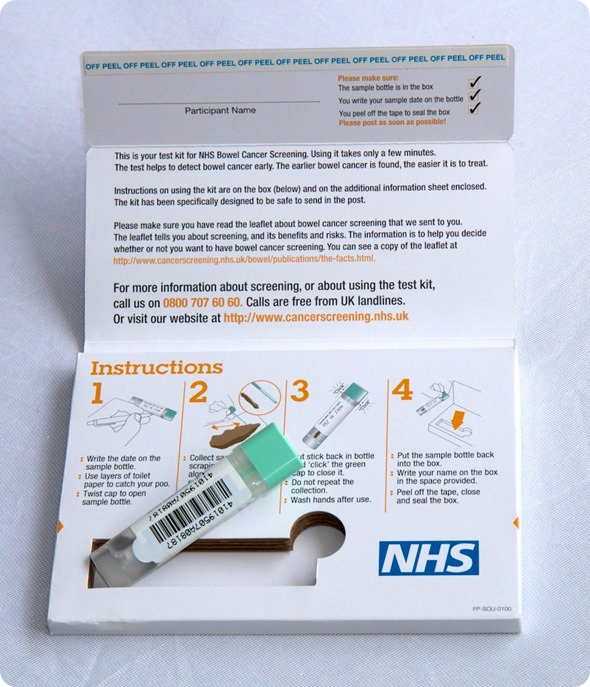
The test requires a small sample of stool collected on a plastic probe which is returned to the NHS Screening Hubs by mail in a small tube. FIT is simpler, easier to use and more hygienic than the current gFOBT and can detect more cancers and pre-cancers.
Can you give an overview of the pilot you carried out?
To ensure FIT was a suitable replacement for gFOBT we compared the performance of both tests in the NHS screening program. Between April and October 2014 we invited over 41,000 subjects to use FIT in place of the regular gFOBT and we compared uptake and outcome with over 1.1 million subjects receiving gFOBT invitation.
Over 50% of the eligible screening population was used in this pilot and they lived in the south, the midlands and north west of England.
The pilot data was analyzed independently by Professor Sue Moss, a Screening Epidemiologist at the Wolfson Institute of Preventative Medicine, Queen Mary University of London.
A detailed statistical, economic and summary report of FIT pilot was then presented in July 2015 to the National Screening Committee who formally recommended it to the NHS in England and to Government in January 2016.
How effective was FIT at increasing screening uptake?
The impact of FIT on participation rates was spectacular! Whilst showing a 7% increase in uptake overall, its major impact was in groups that had hitherto been reluctant to participate.
The group that had failed to participate in the past almost doubled its uptake from 12% to 24%, men aged 60 who were invited for the first time increased uptake by 11% and even those who appreciate the importance of screening increased their uptake to over 90%.
Overall the pilot showed that 290,000 more people would participate in the bowel cancer screening program if FIT were to be adopted.
Why do you think more people are happy to take the new test (FIT)?
The new test was delivered in a simple to open, read and return package. It looked more attractive and professional than the existing test but most of all it was much easier to use and required a single sample and the current test requires two samples on three days. You might well say ‘why would you not do a FIT’!
How important is early diagnosis for the treatment of bowel cancer?
Approximately 97% of bowel cancers caught early (at stage I) will have an average five-years survival rate and most will be cured whilst if caught when cancer has begun to spread (stage IV) then average survival rates fall to 7%.
FIT and gFOBT can also prevent cancer by detecting adenomas (polyps) before they turn into cancer and FIT is many times more effective at prevention because it can detect much smaller quantities of blood.
What impact do you think FIT will have on bowel cancer screening uptake?
The FIT pilot undertaken in England showed a massive increase in uptake which was greater than has been demonstrated in any other screening trial or study.
The uptake is likely to grow since ‘new’ 60 year old participants are likely to maintain their participation in subsequent years. Perhaps the expected increase of 290,000 participants might double after three or four rounds of invitation!
What do you think the future holds for bowel cancer screening tests?
We are already exploring how we might use FIT in a more ‘intelligent’ way. All screening tests assess risk and for bowel cancer, age, sex, cancer family history, some associated diseases and various lifestyle related activities are also predictors of risk.
The assessment of bowel cancer risk using FIT could be enhanced by combining it with some of these personal risk markers similarly to the way we assess the risk of heart disease where we include age, sex and BMI as well as biochemical tests like cholesterol. We might also choose to include the higher risk associated with those who have missed previous screening invitations!
Many DNA markers in blood and feces have been developed but none, as yet, has proven better than FIT for population-based screening. The search continues and new avenues are being explored including looking at the flora of ‘the microbiome’, bacteria which populate our gut, and also the possibility of using breath analysis to detect changes in composition which might be characteristic of bowel cancer. Whilst I expect FIT to be used for the next 10 years I would not like to predict beyond that!
Where can readers find more information?
About Professor Stephen Halloran MBE, FRCPath.
Professor Stephen Halloran is a member of the UK Bowel Cancer Screening Advisory Committee and advisor on population-based CRC screening to many international government health organizations. Stephen is also a medical advisor for Bowel Cancer UK, the UK’s leading bowel cancer research charity and part of the charity’s Critical research gaps in bowel cancer project team.
Professor Stephen Halloran is based in Guildford, Surrey. He developed and directed the NHS Bowel Cancer Screening Programme (BCSP) Southern Hub from its inception in 2006 until his retirement in March 2015. Stephen developed and directed the NHS Guildford Medical devices Evaluation Centre (GMEC) and was Consultant Clinical Biochemist at the Royal Surrey County Hospital.
He is Professor Emeritus (Clinical Biochemistry) at the University of Surrey and continues to have an active role in supporting colorectal cancer (CRC) screening activities worldwide most recently in Canada, New Zealand, Taiwan, The Netherland and other countries of the EU.
Stephen was Editor-in-Chief of the Annals of Clinical Biochemistry, founding editor of www.labtestsonline.org.uk and director of the Surrey MSc in Clinical Biochemistry & Molecular Biology.
Stephen authored many NHS advisory reports on the technical and scientific effectiveness of clinical analyzers. He has published more than 60 recent papers on CRC screening and was the lead author of the European guidelines on colorectal cancer screening (published in 2010). Stephen has a particular interest in factors that influence participation in CRC screening and the scientific, clinical and analytical aspects of faecal immunochemical tests for hemoglobin (FIT).
Stephen is a member of the UK Bowel Cancer Screening Advisory Committee and advisor on population-based CRC screening to many international government health organizations. He founded and chaired the World Endoscopy Organization Colorectal Cancer Screening Committee’s Expert Working Group ‘FIT for Screening’, a group that promotes improvements to FIT and prospers its use in screening programs across the world.
He is a member of the UK Bowel Cancer Screening Advisory Committee and advisor on population-based CRC screening to many international government health organizations. Stephen is also a medical advisor for Bowel Cancer UK, the UK’s leading bowel cancer research charity and part of the charity’s Critical research gaps in bowel cancer project team.
Stephen was awarded an MBE for his services to clinical science in 2010.