Detection of malignant skin alterations is currently aided by optical microscopes such as dermoscopes or optical microscopes. While the latter offers high resolution, it comes with a major disadvantage, just like any other purely microscopic method: it only provides a partial view of the skin due to the low penetration depth.
This makes the non-invasive inspections of deeper skin layers and structures impossible as the images become increasingly blurred with depth due to photon scattering in the tissue.
Our technique, termed optoacoustic mesoscopy, can visualize deeper in tissue overcoming obstacles that have limited microscopy and visual inspection for centuries.
In addition, it offers measurements of inflammatory, allergy, neoplastic and other pathophysiological biomarkers with a simple and fast skin inspection potentially providing physicians with new insights into complex diseases spanning from cancer detection to the assessment of psoriasis or exczema therapy.
Most importantly, optoacoustic mesoscopy operates noninvasively and without administration of exogenous agents and as such is very safe for human use.
Optoacoustic mesoscopy generates ultrasound signals inside tissue following skin illumination by safe light pulses in the visible or the near-infrared spectrum.
The ultrasound signals are generated by a phenomenon called thermo-elastic expansion, due to minute local volumetric increases following the absorption of light by various tissue molecules.
While conventional optical techniques use optical detectors (such as digital cameras, lenses etc.), our method utilizes ultasound detectors that capture a very broad ultrasonic band, from a few MHz to hundreds of MHz.
The use of these broadband detectors allows the formation of optical images with unprecedented resolution and depth.
As a result, we are able to obtain detailed information about the skin morphology, skin microvasculature, inflammatory changes, melanin distribution, blood oxygenation or the metabolic state of tissue. No other imaging method currently offers such rich information profile without using contrast agents.
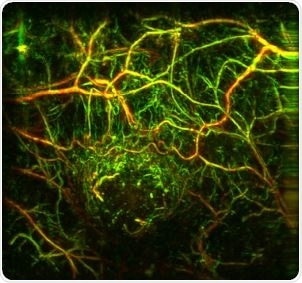
Imaging of tumor vasculature in a mouse model acquired with raster scan optoacoustic mesoscopy (RSOM).
What prompted you to start developing a photonics device for skin diseases?
Although medicine has been traditionally applied in an empirical manner, improving diagnosis, the assessment of therapy and the overall quality of healthcare is strongly associated with progress in technology that enables quantitative, personalized measurements of informative tissue biomarkers.
In addition, technology can standardize the quality of healthcare offered between highly specialized and peripheral centers in rural areas. Even if many skin diseases can be assessed by visual inspection at the dermatologist’s office, these views are often subjective and do not reveal sub-surface information.
As we enter the period of precision medicine, it is critical to offer a more complete and accurate description of skin conditions improving early diagnosis and better assessing symptoms or the effectiveness of therapy.
Overall we are particularly interested in detecting pathological alterations of the skin (e.g. in inflammatory skin diseases or allergies) that affect large populations and have adverse effects on the quality of life. We hope that in this way we will assist dermatologists in diagnosing earlier and better planning and assessing treatment on a per-patient basis.
How are skin diseases traditionally diagnosed and what are the main challenges with current methods?
Until today, skin diseases are traditionally diagnosed by visual inspection of the affected area. In many occasions accurate diagnosis is not possible, and therefore a biopsy and subsequent histological analysis is required.
Although this procedure is the current gold standard for reliable diagnosis and staging it is invasive, slow, and expensive. On the other hand, severity assessment and monitoring of disease progression is mainly done by visual inspection, which only evaluates surface skin features and is subjective.
The absence of sub-surface, three-dimensional information also complicates modern diagnosis and staging accuracy.
Do you think the new photonics device could lead to more accurate and objective diagnoses of skin conditions?
Absolutely; we are convinced that skin disease detection based on optoacoustic mesoscopy can lead to the accurate quantification of biomarkers relating to cancer, inflammation or allergy and significantly complement visual inspection.
We hope that the increased accuracy will reduce the number of biopsies, offer earlier detection, better treatment planning and administration and make the overall disease assessment more objective, in analogy to a blood test which reports numbers.
We have already preliminary data demonstrating that the method is able to produce objective and accurate measurements of key cancer and inflammatory features, such as angiogenesis, vessel dilatation or skin oxygenation.
How exactly does the device use opto-acoustics?
Optoacoustics is a physical phenomenon that indirectly measures optical absorption using ultrasonic detectors. This happens because part of the light energy absorbed is transformed into a minute local heat increase which leads to a local transient volume expansion giving rise to a pressure wave.
By using ultra-fast light pulses we excite a very broad ultrasonic frequency spectrum. This ultrasonic signal is detected in multiple locations on the skin surface and, using tomographic methods, is transformed into a three-dimensional image of optical absorption.
By illuminating light with multiple wavelengths we can build spectral skin images, which further lead to quantifying functional biomarkers such as skin oxygenation and metabolism.
What depths under the skin can the device visualize and what features can the device allow us to see?
Depending on the wavelength and resolution employed, optoacoustic mesoscopy can penetrate up to 5 mm depth attaining resolutions in the 5-50 micron range, although at lower resolution (100— 200 micrometers), optoacoustic imaging can reach more than 2cm of depth.
This performance enables visualization of the entire epidermis, the dermis and beyond. As explained above, the technique can resolve highly diverse contrast ranging from visualizing skin and skin disease morphology (e.g. melanoma, psoriasis, eczema etc.), melanin and melanoma formations, vascular patterns, inflammatory and allergy patterns, skin oxygenation and hypoxia, changes in oxygenation, blood volume and flow and the metabolic state of tissue.
What stage of development is the photonics device currently at?
We have completed a first prototype of the device and have performed pilot studies in humans together with our clinical partners at the Dermatology Clinic (Biederstein Campus) of the Klinikum Rechst der Isar (Prof. Eyerich and Prof. Biedermann).
With the Horizon 2020 EU program investing in this technology, we will be able to develop a superior imaging device that implements spectral illumination, improves the resolution and penetration depth and perform a larger number of measurements to better investigate the diagnostic and theranostic potential of the method.
How much further research will be required before the device can be used in a clinical setting?
We expect to complete the device development and pilot clinical measurements within a time frame of 3 years.
As in any technology, we would require another 2 years to adapt the technology to particular needs and performance required and demonstrate the clinical value. We expect that after this time-frame, optoacoustic skin mesoscopy will be ready for clinical launch.
What do you think the future holds for detecting skin disease?
We aim in delivering an economic, portable and highly performing technology that will be widely accessible by dermatology patients. Our goal is to improve accuracy, quantification and the quality of skin healthcare offered leading to objective and earlier detection and more efficient therapy monitoring.
Where can readers find more information?
The readers can find more information in our publications, as well as on the website of the project for INNODERM, which has received a grant of EUR 3.8 million from H2020, the EU framework programme for research and innovation under the Photonics 21 Public Private Partnership.
About Professor Vasilis Ntziachristos
 Prof. Ntziachristos is a Full Professor and Chair of the Department of Biological Imaging of the Technical University of Munich and Director of the Institute for Biological and Medical Imaging at Helmholtz Zentrum München. He has authored more than 370 peer-reviewed publications and according to Google Scholar he has more than 24,000 citations and an h-index of 73. He has received many awards including the 2013 Gottfried Leibniz Prize, Germany’s most prestigious science award and the Gold Medal from the World Society of Molecular Imaging. He is the editor of the journal of PHOTOACOUSTICS and regularly serves on boards and committees in international societies and conferences.
Prof. Ntziachristos is a Full Professor and Chair of the Department of Biological Imaging of the Technical University of Munich and Director of the Institute for Biological and Medical Imaging at Helmholtz Zentrum München. He has authored more than 370 peer-reviewed publications and according to Google Scholar he has more than 24,000 citations and an h-index of 73. He has received many awards including the 2013 Gottfried Leibniz Prize, Germany’s most prestigious science award and the Gold Medal from the World Society of Molecular Imaging. He is the editor of the journal of PHOTOACOUSTICS and regularly serves on boards and committees in international societies and conferences.