Lynch syndrome is the most common cause of hereditary bowel cancer but carriers are also placed at a higher risk of developing a number of cancers including stomach, ovarian, urological (bladder and kidney) and skin.
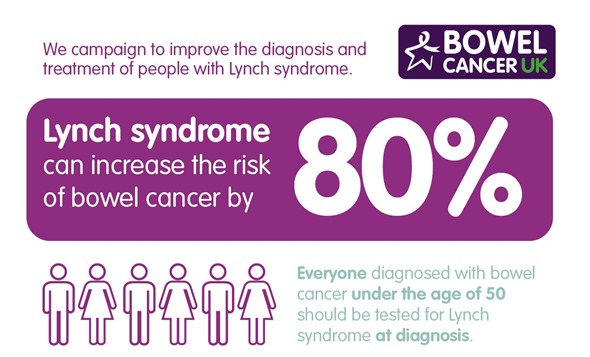
People with Lynch syndrome are often are diagnosed with bowel cancer at a young age, and have a lifetime risk of bowel and/or endometrial (womb) cancer of 60-70 per cent, ovarian cancer of 10-12 per cent.
Fewer than five per cent of people with Lynch syndrome have been identified because there is no systematic testing for Lynch syndrome currently in place in the UK. This has caused variation in clinical practice leading to some people not being offered the test and placed in surveillance.
However the new NICE guidelines which I have developed with others, and are now publically available in draft form, recommend universal testing of all new bowel cancer patients at diagnosis. With this new strategy over 300 bowel cancers are expected to be prevented each year in the UK.
How is Lynch syndrome typically identified? What tests are available?
Clinicians have traditionally used selective criteria to assess and identify individuals who they suspect of having Lynch syndrome. These patients generally have a strong family history of bowel, womb or ovarian cancer that over several generations. Lynch syndrome may be suspected by clinicians if:
- At least two relatives on the same side of the family have had bowel cancer
- A family member developed bowel cancer at a young age (under 50)
- There are cases of bowel and womb cancer on the same side of the family
- Three or more relatives on the same side of the family have had one Lynch syndrome-type cancer
With the new NICE guidelines this process of identification will be simplified by simply testing everyone who has been diagnosed with bowel cancer (at any age, and immediately at the time of their diagnosis). Hopefully we should identify a lot more people who are at risk in this way.
Once Lynch syndrome is suspected testing for Lynch syndrome usually involves a two-step process:
- Molecular screening test - a simple screening test (also known as a molecular test) can be carried out on the patient’s tumor tissue to identify if they are likely to have Lynch syndrome. This test looks for changes in the mismatch repair genes.
- Genetic testing - if changes to the genes are detected in the provisional screening test, patients will be referred for full genetic testing to have their diagnosis settled. This involves a simple blood test and confirms that a change in the gene is present. Usually this takes around 6-8 weeks but in some cases it can take up to a year because of the difficulty in finding the faulty gene.
How is Lynch syndrome inherited and what is the percentage chance that a family member might also have the condition and be at risk for bowel cancer?
Lynch syndrome is caused by a fault in a MMR gene which everyone has two copies of – one from each parent.
If someone has Lynch syndrome it means they have inherited one healthy gene but also one that’s faulty. If that person was then to have a child there would be a 50–50 chance that they will pass on the faulty gene which could then place the child at greater risk of bowel cancer. This is why generations of families can be affected by Lynch syndrome.
Who should be tested for Lynch syndrome?
All people diagnosed with bowel cancer at any age should have the molecular screening test, and the gene test would probably be offered to about 5% of people when they have had this initial test on their tumor biopsies.
If Lynch syndrome is identified, what options are available to reduce the risk of dying from bowel cancer?
While there is no known cure for Lynch syndrome the risk of developing bowel cancer can be reduced by managing the effects of the condition throughout a patient’s lifetime. The risk of bowel cancer can be reduced by:
- Regular colonoscopy
- Aspirin
- Preventative surgery
Placing people with Lynch syndrome in a surveillance program to receive regular colonoscopy is an effective way of preventing bowel cancer in people with Lynch syndrome.
Clinical guidelines by the British Society of Gastroenterology (BSG) recommend that a colonoscopy should take place every 1 to 2 years. It’s important that everyone with Lynch syndrome is placed in a surveillance program to receive regular colonoscopy as this can reduce mortality from bowel cancer by as much as 72%.
Clinical trials have also shown that taking regular aspirin from the age of 45 can significantly reduce the risk of bowel and other cancers in Lynch syndrome carriers by over 50%.
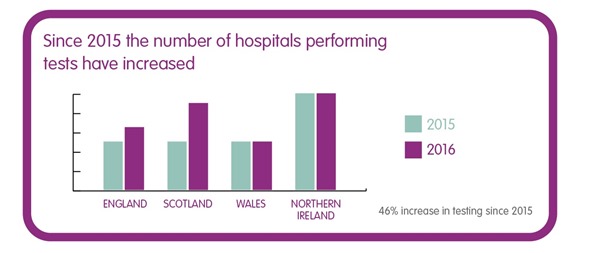
How many hospitals in the UK are testing those under 50 diagnosed with bowel cancer for Lynch syndrome?
In a Freedom of Information request conducted earlier this year by Bowel Cancer UK and the Royal College of Pathologists, it was found that 29% of hospitals across the UK do not routinely test patients under 50 diagnosed with bowel cancer for Lynch syndrome.
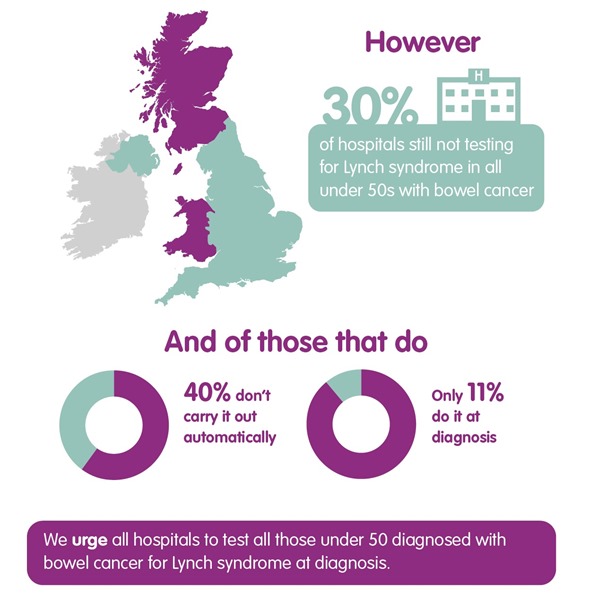
Even those hospitals that do carry out the test, just over half (56 per cent) perform the test automatically as a reflex test as stated in the RCPath guidelines. In many cases, hospitals are even delaying the test until after treatment for bowel cancer with only one in 10 (11 per cent) testing at diagnosis.
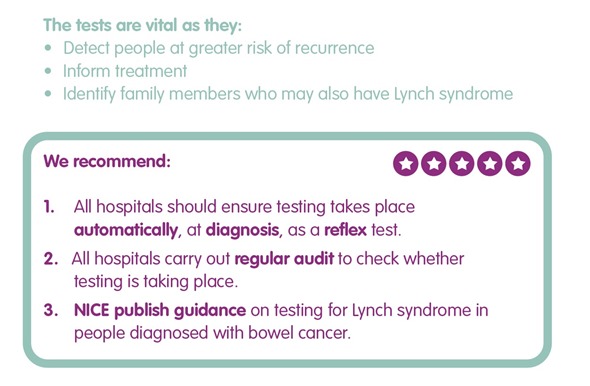
Testing at diagnosis is vital as we know Lynch syndrome can affect treatment options for bowel cancer. There needs to be in place a consistent approach for hospitals that enables this testing to take place automatically, as a reflex test, at diagnosis of bowel cancer, particularly with the new universal testing strategy. This will help reduce variation in clinical practice.
What challenges do hospitals face when implementing the Royal College of Pathologists clinical guidelines and how can these barriers be overcome?
The FOI found that the main obstacles to implementing the guidance for testing of Lynch syndrome are financial, resource and capacity barriers. A lack of NICE clinical guidance for testing was also listed as a barrier by a number of hospitals.
Other factors could be a lack of awareness of the requirement to test or the absence of a specialist gastrointestinal pathologist in some smaller units.
However, we know from formal studies that molecular testing for Lynch syndrome is a cost-effective use of resources. Knowing that a person has Lynch syndrome means that they can be placed in a surveillance program to receive regular colonoscopy. This can help improve patient outcomes by detecting bowel cancer at an earlier stage when it is less costly to treat and has a better prognosis.
What impact could increased testing for Lynch syndrome have?
Increasing testing for Lynch syndrome can help detect more people at greater risk of recurrence, informs treatment options and help to identify family members who may also have the condition and be at risk of bowel cancer themselves.
As Lynch syndrome is an inherited condition knowing if someone does have the condition means that the patient and their family can be offered a surveillance program to receive regular colonoscopy, which can reduce their chance of dying from bowel cancer by as much as 72 per cent.
Where can readers find more information?

About Kevin Monahan
Dr Kevin Monahan (Service lead) spent 3 years working at Cancer Research UK where he completed his PhD in cancer genetics with funding from the Bobby Moore Fund for Bowel Cancer Research, working also at the Family Cancer Clinic at St Mark's Hospital in Harrow.
Currently he leads a familial cancer service called the 'family history of bowel cancer clinic', working closely with colleagues at West Middlesex University Hospital, part of Chelsea and Westminster Hospitals NHS Trust.
Dr Monahan is on the medical advisory board of Bowel Cancer UK, and Lynch Syndrome UK. He is currently continuing his research interests in clinical and molecular aspects of gastrointestinal disease, particularly in the field of endoscopy, colorectal, pancreatic and other GI cancers, GI polyps and other neoplasia.