Theory about the Embryo-Cryo treatment
An interview with Dr Iavor K. Vladimirov, conducted by James Ives, MPsych
Please give a brief overview of current state of assisted reproductive technology and the current applications of embryo cryopreservation versus fresh embryo transfer (ET).
If we were to compare the progression of cryopreservation technology during recent years, we would find that from 2004 to 2013 over a timeframe of a decade, there has been around a 2.5 times increase in the rate of frozen-thawed embryo transfers (FETs) that were reported to the Society for Assisted Reproductive Technology (SART). While the rate of fresh embryo transfers (ET) that were completed was the same.
 This increase in the usage of FETs correlated with a quick growth in the number of live births as compared with fresh ETs. Thus, embryo freezing and thawing efficiency has improved dramatically with widespread use of vitrification vs. the older slow freezing method.
This increase in the usage of FETs correlated with a quick growth in the number of live births as compared with fresh ETs. Thus, embryo freezing and thawing efficiency has improved dramatically with widespread use of vitrification vs. the older slow freezing method.
What benefits are gained from embryo freezing?
Freezing embryos in assisted reproduction is mainly used in order to preserve them, as well as in cases of early progesterone increase during stimulation or to prevent ovarian hyperstimulation syndrome.
In recent years, however, frozen embryos have had another purpose. Paradoxically, many studies have shown that thawed embryo transfer has a higher success rate than that of the fresh, especially in women older than 38.
Studies have shown that the percentage of extra uterine pregnancies and premature births is significantly higher in fresh embryo transfers, compared to FET. Babies born after FET are 90-130g heavier in terms of body weight than those after fresh ET.
Please give an overview of your latest study “Theory about Embryo Cryo-Treatment” and the theory you put forward.
This is the first theory that provides a scientific explanation of the causes and the mechanism for higher success rates of FET. Freezing/thawing can be seen as a way to stimulate the endogenous survival and repair responses in preimplantation embryos.
Many molecular mechanisms are able to explain the increased success rate of ET while using thawed embryos compared to fresh ET in women of advanced reproductive age, the higher miscarriage rate in cases of FET at blastocyst stage compared to FET at early cleavage embryos, and the higher perinatal parameters of born children after FET.
Also, the possibility of advantages arising from the freezing and thawing process described in the theory should enable researchers to rethink the position of cryobiology in reproductive medicine.
How does cryopreservation affect the embryos? What mechanism causes these benefits?
Upon analyzing some Assisted Reproductive Technology studies and results that have not yet been satisfactory explained, we have uncovered evidence that proves that the freezing and thawing procedure has a “therapeutic” effect on the embryos.
Embryos are able to adapt and develop in a large range of cultivation media, showing different gene expression models in different environments. This process causes stress and is known as “hormesis”. If the embryo is placed in slightly unfavorable conditions, it would develop.
However, if the conditions are too unfavorable or toxic, the embryo stops its development and dies. Hormesis is a response on the embryo’s part that induces protective signals. Mitochondrial activity is suppressed below a certain threshold required to initiate implantation during freezing.
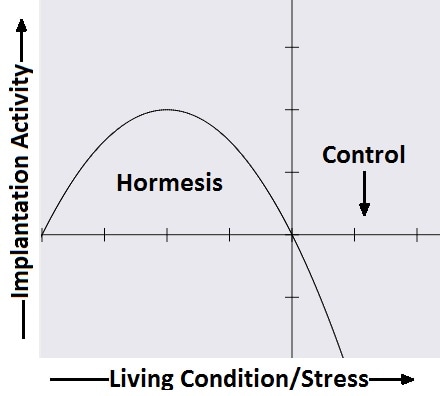
Mechanism of hormesis.
In thawing, there is a rapid recovery of mitochondrial activity in trophectodermal cells (the so-called “jumping effect”), which resembles the physiological processes of the embryo and has a beneficial effect on its implantation.
On the other hand, the freezing/thawing procedure has a detoxifying effect on the embryo through a release of mutated cells of mitochondrial DNA and a partial release of reactive oxygen species (ROS).
How widespread is the practice of freezing/thawing embryos? Are these effects seen in all population groups globally?
A number of studies have shown that in-vitro success rate is higher in frozen embryo transfers, compared to fresh. In fact, some IVF programs have completely stopped using fresh embryo transfers as a whole.
As people age many turn to artificial fertility techniques to assist them in their pregnancy, how is the ratio of live births from FET and fresh ET affected? Why is this?
According to the SART-published success rate statistics in IVF clinics as of 2013, the results showed a significant increase in the live birth rate from FETs after the age of 38 years, compared to that of fresh ET.
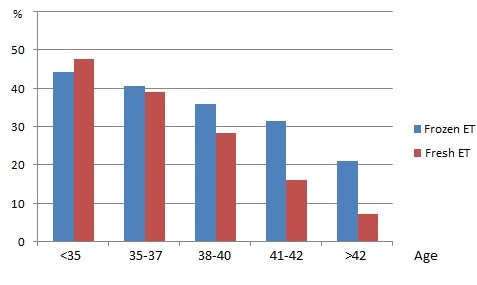
SART-published delivery rate statistics in IVF clinics as of 2013.
This difference is most pronounced in women >42 years of age, as those that underwent fresh ET’s success rate was 7.3%, compared to those that underwent FET with a 21.2% success rate. Other papers also discovered that, with an advancing age in women, the percentage of pregnancies was higher in the cases with FET, compared to fresh ET.
Our theory gives an explanation of those phenomena. The freezing and thawing of embryos reduces the levels of reactive oxidative species and mitochondrial activity, respectively, producing more embryos with a value that is below the threshold of mitochondrial DNA quantities which is necessary to initiate embryo implantation.
Does previous history of childbirth or miscarriage affect the results this technique?
There was an increased risk of miscarriage after FETs versus fresh ET among women younger than 38 years, but when transferring embryos of good quality, the risks of pregnancy loss were similar between fresh and frozen cycles. On the contrary, in women older than 40 years, the risk of miscarriage was lower when transferring frozen embryos versus fresh.
How are the differing stages of development affected by cryopreservation? Is there a best time to cryopreserve or are there similar levels of live full term births?
Some studies have found that blastocyst FET is associated with a 14% higher risk of spontaneous abortions, compared to FET of early cleavage stage embryos. Nevertheless, I would recommend that the embryos should be cultivated to blastocyst stage to determine the embryo potential and eliminate those with serious genetic defects.
On the other hand, through freezing the blastocysts, the benefits from freezing/thawing can be maximized. Last, but not least, frozen embryos in blastocyst stage can be thawed and transferred when the endometrium is ready to accept them after finding of the so-called “implantation window”.
Do children born after FET suffer ill health effects of complications as a result of this procedure? How does this compare to fresh ETs?
In the studies conducted on children born after embryo transfer, no results have been found to show an increase in congenital anomalies or developmental problems in children.
So, children born after FET are not different from those born after a fresh ET. On the contrary, studies show that the percentage of children born with Down syndrome is lower after FET, compared to fresh ET.
What disadvantages are there to using FETs as compared to fresh ET?
The disadvantages are not that many, but they still exist. The survival rate of embryos after freezing and thawing is 95-96%. The risk for having placenta accrete and an excessive birth weight baby seem to be increased in FET as compared to fresh ET.
What would you like to see as the future of assisted reproductive technology?
There is a thought from Mahatma Gandhi “A nation's greatness is measured by how it treats its weakest members”. I would like to paraphrase it in the following way: “The level of development of human society can be measured based on how it cares for its unborn children, i.e. the embryos”.
Today, with the assistance of reproductive technologies, we produce a large number of embryos, however only a small part of them result in the birth of a baby. I would like of us to think of every embryo that we have created as a separate person, and to take care of it, so that a happy baby can be born.
Where can readers find more information?
More information can be found in our article “Theory about the Embryo Cryo-Treatment” in the “Reproductive Medicine and Biology” journal published by the Japan Society for Reproductive Medicine, Volume 16, Issue 2, 118–125 DOI: 10.1002/rmb2.12027 (http://onlinelibrary.wiley.com/doi/10.1002/rmb2.12027/full), or on the SBALAGRM-Sofia website (www.ivf.bg).
About Dr. Iavor K. Vladimirov 
Dr. Iavor K. Vladimirov is the founder and medical director of the Sofia IVF clinic (“SBALAGRM-Sofia”). He is an honorary lecturer at “St.Kliment Ohridski” University in Sofia.
Dr. Vladimirov was one of the participants in the IMPORT & IPD-EXPORT Study Group, which analyzes the objectivity of ovarian reserve tests. He has made a significant contribution in the ERA-RCT study, which defines the advantages of the implantation window (ERA) test. This report has been honored by the Society for Reproductive Endocrinology and Infertility during the 72nd annual ASRM meeting as a Prize Paper for 2016.
Dr. Vladimirov is one of the authors of “Theory about the Embryo Cryo-Treatment” in the “Reproductive Medicine and Biology” journal published by the Japan Society for Reproductive Medicine.