Antibiotics are a boon to mankind and as more and more microorganisms are developing a resistance to these drugs, researchers are delving deeper into the mechanisms of this resistance. It is a commonly held view that once begun, a course of antibiotics should be completed to prevent the emergence of resistance among the microbes.
Now Martin Llewelyn and colleagues from Brighton and Sussex Medical School, the University of Oxford and other institutions have come up with a new analysis that differs from this “commonly held” notion. They find that there is no connection between exposure to antibiotics and development of antibiotic resistance in large populations as well as in individual patients. Thus, unnecessary antibiotic use should be curbed to prevent resistance. Their analysis is published in the British Medical Journal.
Even the World Health Organization has maintained the message that failing to complete a course of antibiotics may invite the risk of antibiotic resistance. The material spread at the Antibiotic Awareness Week 2016 WHO advised patients to “always complete the full prescription, even if you feel better, because stopping treatment early promotes the growth of drug-resistant bacteria.” This message has been part of national campaigns worldwide since antibiotic resistance is such a global menace. Even secondary school students in United Kingdom are being taught the importance of completing a full regimen of antibiotics.
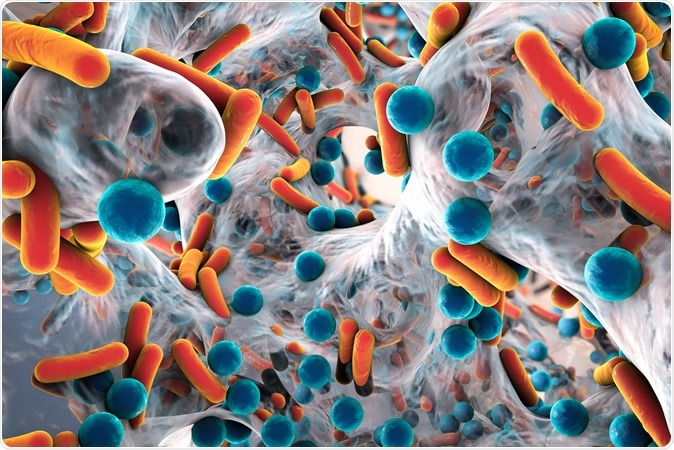
Illustration of biofilm of antibiotic resistant bacteria, closeup view. Rod-shaped and spherical bacteria. Escherichia coli, Pseudomonas aeruginosa, Mycobacterium tuberculosis, Klebsiella, Staphylococcus aureus, MRSA. Image Credit: Kateryna Kon / Shutterstock
Alexander Fleming who developed Penicillin in his Nobel acceptance speech in 1945 had envisaged a time when if a man took inadequate amount of penicillin for a strep throat infection, he ends up transmitting the resistant strain of the bacteria to his wife who succumbs to the infection. He advised that if one uses penicillin, he or she should take “enough”. This is interpreted as for an adequate duration of time to prevent development of antibiotic resistance. The advice now is being slightly changed. It says to take the antibiotics exactly as prescribed to avoid long term unnecessary use of antibiotics. This means “enough”, neither too short a duration nor too long.
Scientists have explained the mechanism of development of antibiotic resistance.
Target selected resistance - When a microbe multiplies within the host it leads to infection. These microbes may undergo genetic mutations that may make them deadlier and resistant to antibiotics. These genetic mutations are seen to be accelerated in case of inadequate dosing of the antibiotics or when a single drug is used to kill the microbe. Tuberculosis, HIV, typhoid, malaria and gonorrhoea are notable infections that develop resistance in this manner.
Collateral selection – There are several bacteria types that live harmlessly within the gut or other mucus membranes. During antibiotic treatment for other infections, these harmless bacteria genetically mutate to become resistant and cause infections. Their mutations are passed on to other strains of the bacteria leading to antibiotic resistance. Organisms that show this type of resistance include Methicillin Resistant Staph aureus (MRSA).
Researchers have seen that most of the antibiotic resistance now does not come from the first type of resistance selection or target selection. This means the second type is more common. This also means that longer the duration of the antibiotic use, longer the time the harmless bacteria in the gut gets to develop resistance and pass it on to the other strains and species of bacteria. These harmless bacteria are called “opportunistic pathogens” which means they become dangerous only at certain times i.e. antibiotic use, immunosuppression etc.
In this new work, researchers have suggested optimum usage of antibiotics as the key to prevent resistance. They write that hospitals already practice this by repeatedly testing the patients and modifying the dosage and duration of the antibiotic use. Once out in the real world, patients may not be able to undergo repeated tests to adjust their antibiotic use. Thus, it is easy to follow the advice of “completing the course” that has been determined from previous experience and evidence. Authors of the study called for more such studies to check on how long antibiotics can be safely and effectively taken to prevent emergence of antibiotic resistance.