An interview with Brian Smith, conducted by James Ives, MPsych
Can you please give an overview of perioperative practice? How does it differ from generalised practice?
Perioperative practice is quite a specialised area focused on patients who are undergoing surgery. Patients come to theatre for a reason, usually to have an operation or procedure that will correct a condition or perhaps alleviate discomfort.
In general nursing, on the wards, the holistic patient needs are taken care of before and after surgery. Vital signs such as blood pressure, heart rate, and respiration rate are recorded and documented in the patient notes.

Perioperative refers to three phases of care; pre-operative is where tests might be undertaken or consultations take place with the anesthetist and the surgeon. The second phase is the intra-operative phase where the patient is transferred to the anesthetic room and given medication to sleep or light sedation during a procedure.
Patients are then transferred to the operating room where the procedure is performed. The third phase is post-operative where expert staff will support the patient coming around from their operation. This is also known as the recovery room.
What skills are learnt in training for perioperative practice?
The skills in perioperative practice are quite specific and focused around the activity areas of Anesthesia, Surgery, and Recovery. The highly specialised and fine-tuned skills are applied in a controlled manner.
During the anesthetic activities, practitioners assist with providing individualised care in the anesthetic room. Communicating effectively with the patient, the anesthetist and the rest of the team will ensure all specialist equipment such as the anesthetic machine; intravenous equipment and airway management are available and fully functional.
Staff working in surgery will ensure all surgical instruments, diathermy machines, lasers, endoscopes and robots are working correctly before the patient arrives. Surgical items such as swabs are counted before, during and after the operation.
Knowledge of each surgical procedure and human anatomy is essential for anticipating any potential problems during the operation. In addition, the anesthetic and surgical staff will work collaboratively to position the patient on the operating table under the guidance of the surgeon and anesthetist.
Patients in the operating department are constantly monitored for their heart rate, blood pressure, temperature, etc. The perioperative staff keep a close eye on the patient's physiology to ensure they are not experiencing any pain, or discomfort.
Their vital signs are important in assessing how they're reacting to the surgery. This close monitoring is a continuous process throughout the patient’s perioperative journey into recovery.
How do the skills learnt for the perioperative practice transfer to other high intensity areas such as the intensive care unit and emergency departments?
Perioperative practice skills can extend across different specialist areas. Many people who have worked in perioperative practice have moved into other perioperative surgical specialties, critical care, and intensive care or emergency department roles.
Application of care in different departments or roles allows practitioners to understand what brings people into hospital, or perhaps for emergency care.
In emergency departments, you might find some of the perioperative team looking after the critically ill patients who may have been in a road traffic, industrial or home incident.
Perioperative staff also participate in emergency response or critical incident teams which are based out of the hospital location, caring for injured or distressed patients. You also find the same skills prevalent in the military, where practitioners might be part of emergency teams transporting injured patients to medical centers.
How is perioperative practice different in a military setting? What additional skills are required?
While there are similarities in how patients are treated in hospitals, arguably more situational awareness might be necessary in military settings. It is important in all perioperative settings that we communicate effectively, conveying messages clearly and succinctly when under pressure.
Although perioperative environments can be pressured, the competence and professional behaviour of the team keep this controlled. The World Health Organisation Safer Surgery Checklist ensures the surgical team know what professional skills will be applied in practice.
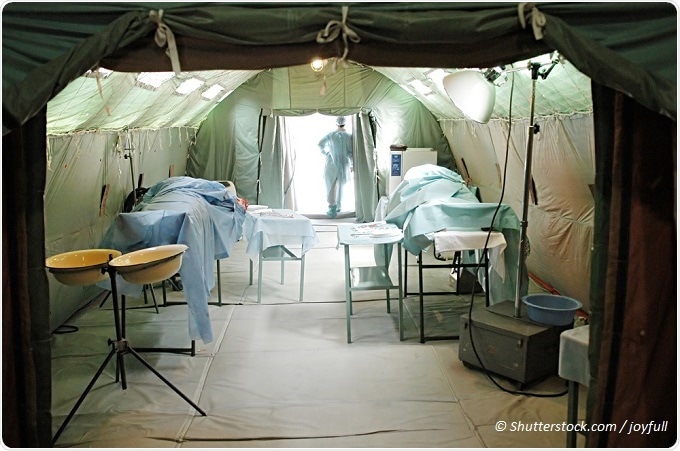
In military settings when you're working out in a rural location, established teams will be present even when working in a temporary medical centre. In this particular scenario, not all equipment might be in the same place, or in the same location, so what you have to do is know what's in your Medipacks, or in the sterile instrument trays.
When working with vulnerable adults and children what special considerations are taken into account by the perioperative staff?
It is important to adhere to Safeguarding policies and practices when caring for vulnerable patients who enter into the perioperative environment. We must promote the patients’ wellbeing, especially for those who may have difficulty in protecting themselves.
Showing compassion in practice gives you a chance to exercise enhanced communication skills and to provide high quality patient care. Caring for dementia patients or any patient with particular needs requires one practitioner to take the lead in the communication.
Perioperative practice is a very busy environment, and sometimes you might have two or three things all happening at the same time. You might have the practitioner talking directly with the patient, but some background noise or people talking might confuse their state of mind, making it much harder for them to make a decision.
Some people will be very sensitive to the way you say things or the way you approach them in your bodily mannerisms as well as language.
Communication should be considered and crystal clear to avoid upset or confusion in the care perioperative staff are about to deliver to the patient. When approaching a patient, you must always ask for their permission before performing any procedures.
For example, applying ElectroCardioGram (ECG) or taking a blood pressure reading requires the placement of ECG dots on the patient’s chest, or holding their arm while you apply the blood pressure cuff. It's not an automatic thing that you can go ahead and do.
If practitioners have any particular concerns when caring for adults or children, they should contact the safeguarding lead in the department for advice and support.
Is special training given to help with practitioners’ interactions with vulnerable adults and children?
We're starting to see more of an awareness of patient vulnerabilities introduced into basic training. Staff undertake yearly updates in safeguarding training with some practitioners developing a wider understanding in how we communicate and care within the perioperative environment.
The University of Derby Online Learning offers a completely online top-up course for perioperative practice. Please give an overview of the course, what is covered?
The University of Derby Online Learning (UDOL) BSc (Hons) Perioperative Practice Top-up degree is aimed at taking a global perspective of perioperative education, looking at how we address the three main areas of perioperative practice.
The course design allows students to step on and off with some perioperative practitioners perhaps deciding to undertake a module as part of the CPD requirements. Others may undertake the full course and look at the international perspective on safer surgery and contemporary anesthesia and surgical techniques.
We show how anesthesia techniques have changed; we explore new medication and research that influences twenty first century surgery as well as how different types of surgery advantages and disadvantages are debated.
We also look at perioperative practice in different countries where there is less equipment and financial capital available to support the same quality of patient care.
We also use advance-teaching techniques in a new virtual platform to support students in developing their skills and reflective thinking when treating patients. Our virtual hospital has virtual patients waiting for students to care for them when entering the virtual perioperative environment.
Students are also asked to consider the patient’s medical history, the listed operation and make correct decisions for each patient. Decisions are simulated showing outcomes and sometimes consequences!
We are also fortunate to have a two day residential for students to refine and strengthen their skills and knowledge in perioperative workshops. Working collaboratively with medical colleagues and medical company representatives they can critically look at new equipment, research, and surgical techniques.
Our virtual patients will be physically present to share their view on the care given in the virtual theatre.
It's an all-inclusive package that can be studied 100% online and we hope it will build people's knowledge and insight into perioperative practice.
This course is also currently the UK’s first and only online Perioperative Practice BSc (Hons) Top-up degree to be endorsed the Association for Perioperative Practice (AfPP).
Who are the Association for Perioperative Practice (AfPP)? What signification does their accreditation grant to this course and what relationship is there between them and the University of Derby Online Learning?
The Association for Perioperative Practice (AfPP) is an important organisation in developing standards, practice, and education in safe surgery. The collaborative activities of AfPP with other professional bodies such as the College of Operating Department Practitioners and the Perioperative Care Collaborative afford the University of Derby course to be in the vanguard of perioperative advancement.
The Association’s commitment to perioperative education is commended and strengthens what we delivery at UDOL. AfPP also provide professional advice to perioperative practitioners, which will be extended to the students studying on the top-up degree.
I think the AfPP's involvement has made a tremendous difference, not just to the University of Derby Online Learning but to all perioperative programmes providing guidance and support in meeting the needs of future students and their patients.
Who is the course aimed at? What are the prerequisites for entry onto the course and when are the intakes of new students?
This course is a top-up degree for perioperative practitioners with 240 Higher Education credits. Some practitioners may have English National Board qualifications, or NVQ Levels 3 in Operating Department Practice, or a 752 City and Guilds qualification. Each applicant will meet the online tutors and ensure they have the entry points or equivalency requirements.
Students joining the course will be working in the perioperative setting, this might include endoscopy, day case suites, a field hospital, or it could be on a Mercy Ship. Upon successful completion of the course, the individual will be awarded with a BSc (Hons) in Perioperative Practice.
It's open to a global audience, where students can study this course part-time, 100% online. Students also have the opportunity to start this course in January, May or September.
Why would a student looking to move into a more applied area of healthcare choose perioperative practice over other clinical areas of development?
Perioperative practice gives newly qualified students an opportunity to practice nursing skills in a more profound way. They can care for people who require an operation. That means that they have to draw on every single nursing skill they have, to think about how they apply compassion in practice to deliver the very best in care to a patient who's unconscious. We become the patient's advocate.
In the post-anesthetic recovery room, you get a chance to know your patient as they are coming around from anesthesia. Effective communication is fundamental to ensuring that they understand what's happened to them, and gives you a chance to monitor their ability to respond to oral command, before discharging them to the ward.
I think it's a place where you can exercise your full range of technical and soft communication skills, alongside the internal values of why you came into nursing or operating department practice in the first place. It's about making a difference to the patients’ well-being.
Where can readers find more information?
For further information, listen to the University of Derby Online Learning’s recorded webinar; It is about one hour long providing the full programme information.
Introducing the online Perioperative Practice course
You can also contact the university for further information, or you can contact the Association for Perioperative Practice (both links below), who are actively promoting this program.
https://www.derby.ac.uk/online/course/online-perioperative-practice-bsc-top-up-degree-course-program
https://www.afpp.org.uk/home
Equally, those who wish to contact the programme team, they are very welcome to contact myself or Vicky Cockerill at the University of Derby.
We'll give you a very personal and heartfelt perspective on this programme.
Brian Smith - [email protected]
Vicky Cockerill - [email protected]
About Brian Smith
Brian Smith has been a Perioperative Practitioner for thirty years and has contributed significantly to the development of Operating Department Professions. His portfolio of work includes establishing perioperative standards, clinical education, co-designing and delivery of perioperative Higher Education. He is an award-winning, energetic and highly motivated individual with a strong track record of leading enhanced learning in vocational, further and higher education settings at senior level. Brian qualified as an Operating Department Practitioner in 1987, and graduated from Lancaster University with a bachelor's degree in Organisation and Management Studies in 2004, He went on to earn a Post-Graduated Certificate in Education, and in 2008 completed a Masters in e-Learning Education at Edge Hill University. Aside from his Perioperative CPD activities, he is studying a PhD to understand learner behaviour and ontological needs in the learning experience.
In 2012, Brian was awarded the prestigious Higher Education Academy National Teaching Fellow for excellence in teaching and learning for developing inspiring and innovative new models of learning. Brian has an extensive experience in authoring articles, chapters, and books in perioperative education alongside his previous AfPP tenure as the editor for the Journal of Perioperative Practice. Today, he continues to write, and review for the journal alongside his clinical practice and higher education teaching roles.
He has a keen interest in organisational/individual behaviour with a dedicated passion to increase skills and knowledge in the workplace. In his coach/consultant portfolio, he shepherds senior perioperative practitioner in their leadership behaviour, skills, and know-how in promoting safer surgery. He is also a board member of the Association for Perioperative Practice.