Sep 28 2017
Experts from United European Gastroenterology (UEG), presenting at the European Digestive Cancer Days (EDCD) Conference in Prague today, are calling on European governments to focus their efforts on developing early diagnosis techniques, in order to save thousands of lives from digestive cancers including a more targeted approach to ensure at risk patients don’t ‘slip through the early-detection net’.
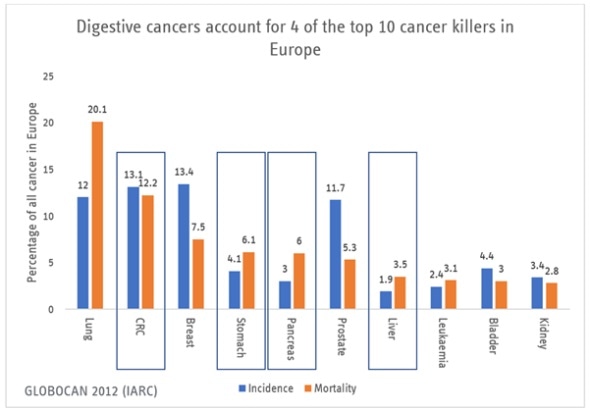
Digestive cancers account for 3 of the top 5 European cancer killers, 23.4% of European cancer incidence and 30.1% of European cancer deaths.
Currently, of the 5 primary digestive cancers, only colorectal cancer (CRC) is screened for and whilst some significant progress has been made in CRC screening in many European countries, early detection of other digestive cancers is still not sufficiently developed, even in high risk patients.
Experts, legislators and patient organizations from across Europe are meeting at the EDCD to present and discuss new developments and research in digestive cancer screening and early detection and will be calling upon governments to focus their efforts on developing specific screening and early detection techniques.
“Today, we are recommending that European governments focus their efforts on improving early detection of digestive cancers by funding and encouraging research in four specific areas; to give at-risk patients the best possible chance of survival. Public health authorities also need to think smarter when delivering screening, including looking at opportunities to screen for more than one cancer at the same time and using new cancer profiling techniques as they become available.” says UEG’s Prof Thierry Ponchon.
UEG is highlighting specific areas for review in digestive cancer screening which they claim could not only improve outcomes but once developed could be straightforward to implement, such as:
- Look to the future to implement faecal microbiota screening (FBS) to predict colorectal cancer (CRC) before it develops. Early studies show that gut microbiota-based prediction is more accurate than the current faecal occult blood test, with the potential to predict CRC before it develops rather than just detect its indicators this is a promising prospect for the future of CRC screening, once further research shows this is proven on a population level.
- Look to screen patients with heartburn or acid-reflux, using the Cytosponge™ or ‘pill on a string’ within the doctor’s practice, to increase early detection of Barrett’s oesophagus - an early precursor to oesophageal cancer. Experts report that existing screening methods for oesophageal cancer are expensive and ineffective, with evidence from the United States showing that only about 7% of people with oesophageal adenocarcinoma are detected through existing endoscopic screening approaches. However, evidence of the use of an affordable, easy, non-invasive test known as a ‘pill on a string’ has shown to be safe, preferable and accurate and if proven on a population basis, should be widely adopted.
- Microbiota screening in alcohol dependent patients at risk of liver cirrhosis and hepatocellular carcinoma (HCC) to determine levels of cancer-protecting short-chain fatty acids (SCFAs). Research indicates that microbiota profiling in alcohol-dependent patients could determine whether the patient’s gut is lacking cancer-protecting SCFAs and could more effectively verify the likelihood of liver cancer developing.
- Gastric cancer screening should be implemented alongside CRC screening in European countries with an intermediate incidence (10 > 100,000). New evidence presented at the EDCD shows, for the first time, that screening for gastric cancer in at least 14 European countries with an intermediate incidence rate would be cost effective if combined with a pre-scheduled colonoscopy for CRC. There is currently no screening provision for gastric cancer in any European country.
Despite the significance of digestive cancer incidence and mortality, progress in establishing digestive cancer screening lags behind breast and prostate cancer and UEG expert, Monique van Leerdam concludes:
whilst we are making good progress in colorectal cancer screening, we need to focus research on developing new targeted opportunities for screening in all digestive cancers and ensure that we give every patient, especially those at higher risk, the opportunity for earlier intervention – it could save many more European lives.