Nov 17 2017
Utilizing an ‘electronic nose’ could be an effective and affordable screening method for the diagnosis of pancreatic cancer, new research suggests.
In research published in the latest edition of the UEG Journal, Scientists in Finland demonstrated that there is variance in the volatile compounds found in the urine of pancreatic cancer patients to that of healthy controls. Research was then undertaken to assess whether FAIMS (Field Asymmetric Ion Mobility Spectrometry) technology could effectively differentiate between pancreatic cancer patients and healthy individuals as a tool for screening.
FAIMS has recently emerged as a new tool for biomolecular analysis, allowing researchers to distinguish between molecules. The technique is affordable (each test costs approximately €20), non-invasive and it is estimated that up to 20 urine samples could be analyzed every hour. When detecting pancreatic cancer and pancreatic pre-malignant lesions, the FAIMS test resulted in a sensitivity and specificity of 85% and 75% respectively.
“The aim is to now improve the sensitivity and specificity of FAIMS technology for pancreatic cancer to 90%” explained researcher Doctor Samuli Nissinen, a specialist in gastroenterology and internal medicine. “We are refining our methods to reach these results, and further tests will soon be undertaken to collect new data”.
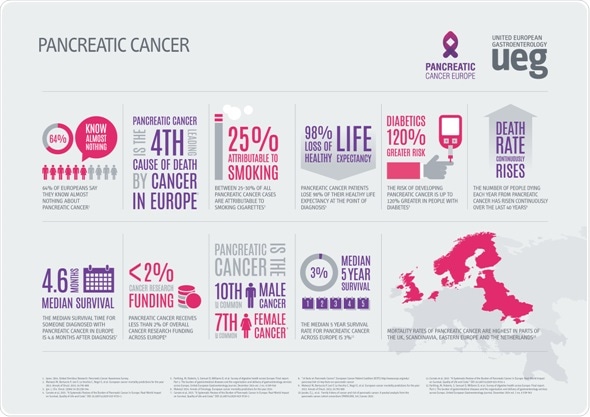
The number of deaths from pancreatic cancer in the EU is expected to overtake those of breast cancer within the near future, meaning that pancreatic cancer will become the third leading cause of death from cancer in the EU. The median survival time for someone diagnosed with pancreatic cancer in Europe is just 4.6 months, with patients losing 98% of their healthy life expectancy at the point of diagnosis.
“The number of people dying each year from pancreatic cancer is rising” adds Doctor Nissinen. “Despite its severity, screening the entire population for the disease is not currently plausible. We do believe that FAIMS has the potential to be a screening tool for pancreatic cancer in high-risk groups, such as people with new onset diabetes, pancreatitis and those who have a family history of pancreatic cancer. However, further research is needed to achieve a 90% accuracy”.
Calls for more research funding across the EU
Meanwhile, over 1,800 digestive health specialists from 99 countries have signed a pledge to call on the EU and its Member States to fund more pancreatic cancer research across Europe. Despite appalling patient outcomes, pancreatic cancer receives less than 2% of overall research funding throughout the continent. Professor Matthias Löhr, UEG pancreatic cancer expert, explains “Pancreatic cancer should be treated as a medical emergency. There is often a lack of awareness and an ignorance towards pancreatic cancer from all parties involved, including physicians and policy makers. We urgently need more research, more awareness, and a policy supporting the speedy diagnosis and treatment for patients”.
To help support this message, increase research and identify the tools for early patient diagnosis, UEG have launched a campaign named #Voice4PanCan.
Pancreatic Cancer: Stuck in the 1970s