Researchers at the Salk Institute have found a way to convert the cells in open wounds into new skin cells, potentially eliminating the need for plastic surgery in the treatment of large wounds.
"Our observations constitute an initial proof of principle for in vivo regeneration of an entire three dimensional tissue like the skin, not just individual cell types as previously shown," says senior author Juan Carlos Izpisua Belmonte, who adds that this could be useful not only for helping skin repair but for guiding in vivo strategies in other human pathological situations.
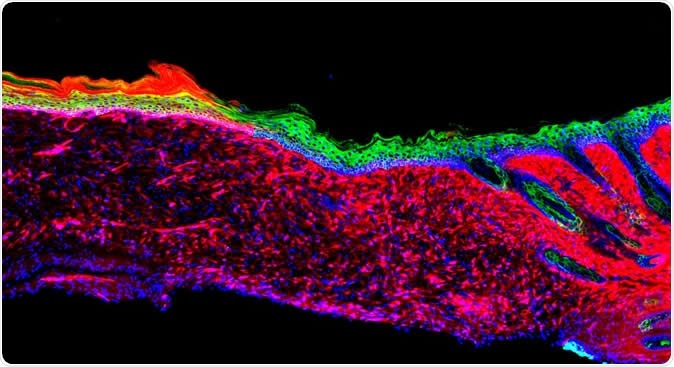
The image represents the first proof of principle for the successful regeneration of a functional organ (the skin) inside a mammal, by a technique known as AAV-based in vivo reprogramming. Epithelial (skin) tissues were generated by converting one cell type (red: mesenchymal cells) to another (green: basal keratinocytes) within a large ulcer in a laboratory mouse model.
Typically, cutaneous ulcers are treated by transplanting existing skin over the wound, but when an ulcer is very large, it can be difficult to graft sufficient amounts of skin. When this problem arises, researchers can isolate skin stem cells from the patient and culture them in a lab before transplanting them. However, this process is time consuming, which can risk the patient’s life, as well as not always being effective.
The researchers of the current study knew that an important step in wound healing is the movement of basal keratinocytes into the wound. These are stem-like cells that are precursors to all the various types of skin cells. However, very large wounds that no longer have multiple skin layers do not have these precursors, and the skin cells that do grow in the area are generally involved in inflammation and wound closure rather than skin repair.
Now Izpisua Belmonte and team have managed to identify four “reprogramming factors” that can convert these existing cells into basal keratinocytes. When they applied the four factors to skin ulcers in mice, the ulcers rebuilt healthy skin within 18 days. Eventually, the skin expanded and connected with nearby skin, even when the ulcers were large. At three and six months, cellular, molecular and genetic analyses showed that the reprogrammed wound cells were behaving like healthy skin cells.
Next, the team plans to enhance the technique and test it in further models of ulcers: "Before going to the clinic, we have to do more studies on the long-term safety of our approach and enhance the efficiency as much as possible," says co-author Masakazu Kurita.
Citation: In vivo reprogramming of wound-resident cells generates skin epithelial tissue, Masakazu Kurita, Toshikazu Araoka, Tomoaki Hishida, David D. O’Keefe, Yuta Takahashi, Akihisa Sakamoto, Masahiro Sakurai, Keiichiro Suzuki, Jun Wu, Mako Yamamoto, Reyna Hernandez-Benitez, Alejandro Ocampo, Pradeep Reddy, Maxim Nikolaievich Shokhirev, Pierre Magistretti, Estrella Núñez Delicado, Hitomi Eto, Kiyonori Harii & Juan Carlos Izpisua Belmonte | Nature (2018) https://doi.org/10.1038/s41586-018-0477-4, https://www.nature.com/articles/s41586-018-0477-4