CDx Diagnostics, an innovator in computer-synthesized, three dimensional tissue analysis for the early detection and surveillance of Barrett’s esophagus, today announced new data for WATS3D, or Wide Area Transepithelial Sampling with 3D Tissue Analysis, demonstrating the clinical significance of crypt dysplasia as an important risk factor for progression to high-grade esophageal dysplasia or esophageal cancer.
Dr. Nicholas Shaheen, Chief, Division of Gastroenterology & Hepatology University of North Carolina at Chapel Hill is presenting the data today in a Presidential Plenary session at ACG 2018, the annual meeting of the American College of Gastroenterology, taking place October 5 -10 in Philadelphia.
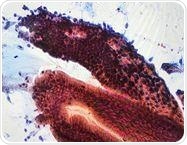
WATS Computer Synthesized En Face View of Crypt Dysplasia. Credit: CDx Diagnostics
Detecting still harmless, but pre-cancerous dysplasia can prevent the development of esophageal adenocarcinoma, the most rapidly growing cancer in the U.S., and one of the most fatal.
Accurately identifying which chronic heartburn patients who develop Barrett’s esophagus have also progressed to dysplasia can have an important impact on patient care.
The clinical significance of dysplasia involving crypt cells has not been well understood due to limitations in detecting crypt dysplasia by conventional biopsies. The data reported today suggest that samples obtained and analyzed with WATS3D allow detection of this condition.
Most importantly, the data also suggest that crypt dysplasia is something we should wish to detect, because it has a higher risk of progression to high-grade dysplasia or esophageal cancer compared to non-dysplastic Barrett’s. Together, the data suggest that WATS3D provides information that forceps biopsy cannot.”
Dr. Nicholas Shaheen
Barrett’s esophagus (BE) occurs when the normal epithelial lining of the esophagus is replaced by goblet cells that are typically found in the lower gastrointestinal tract.
Patients with BE have an increased risk of developing esophageal adenocarcinoma (EAC), a cancer that attacks 17,000 people in the United States each year – of which 16,000 will die from.
Given this risk, it is recommended that patients with BE undergo periodic surveillance endoscopy to monitor for pre-cancerous changes to the esophageal lining.
While non-dysplastic BE (NDBE), low- or high-grade dysplasia (LGD or HGD, respectively) can be diagnosed using standard biopsy criteria, morphologic changes that fell between NDBE and LGD were traditionally classified as indefinite for dysplasia and often grouped with NDBE due to the inability to distinguish dysplasia involving crypt cells (which are located below the epithelial cells) from esophagitis resulting from uncontrolled reflux.
Due in part to the inability to accurately diagnose crypt dysplasia (CD), its clinical significance has not been well understood.
The study results presented today are the first to show that WATS3D enables accurate diagnosis of CD as a distinct histology; they also show that CD is a risk factor for HGD and EAC and that progression rates from NDBE and LGD to HGD/EAC detected with WATS3D are similar to those obtained using traditional forceps biopsies.
What has been under appreciated by clinicians is how incredibly effective the WATS3D computer-assisted analysis and neural network program is at helping pathologists detect dysplasia and, most notably, its earliest form, termed crypt dysplasia.
The WATS 3D technology allows pathologists to ‘put into focus’ atypical lesions that would otherwise be considered indefinite.
The results of this study prove, for the first time, that early dysplastic lesions are clearly important to detect because of their now established increased risk of neoplastic progression. Thus, computer-assisted pathologic detection of these lesions will undoubtedly improve patient care.”
Dr. Robert D. Odze, Harvard Medical School
The study reported at ACG 2018 followed 4,512 patients who had two WATS3D assessments six months apart. Patient-years (pt-yrs) were calculated by multiplying the mean period of follow-up by the number of patients with each type of histology.
Of 4,512 patients, 4,049 with NDBE at baseline were followed for an average of 1.4 years between WATS3D assessments (5,736 pt-yrs) and 380 with NDBE at baseline were followed for an average of 1.25 years between assessments (475 pt-yrs). An additional 83 patients had LGD at baseline WATS3D and were followed for a mean of 1.25 years (103.7 pt-yrs). Key findings from the study include:
- 19 of the NDBE patients followed for 1.4 years experienced progression to HGD/EAC, for a rate of 0.33%/pt-yr.
- 10 of the NDBE patients followed for 1.25 years experienced progression to HGD/EAC, for a rate of 2.1%/pt-yr.
- 8 of the LGD patients experienced progression to HGD/EAC, for a rate of 7.7%/pt-yr.
- The overall rate of progression from WATS3D-determined CD to LGD/HGD/EAC was 9.9%/pt-yr, which is comparable to the rate of progression from biopsy-confirmed LGD.
- Results show that a finding of NDBE or LGD on WATS3D predicts progression to HGD/EAC at rates that are comparable to or higher than the reported risk of progression when these histologies are determined by biopsy.
- For patients with BE, CD or LGD at baseline, the trend for progression to HGD/EAC was statistically significant.
“These results highlight the clinical benefits that WATS3D provides with respect to accurate surveillance of esophageal changes in patients with BE,” said Mark Rutenberg, Founder and CEO of CDx Diagnostics.
“We believe these data highlight how WATS3D provides physicians and patients with accurate and critical information that can inform the management of BE and help preempt esophageal cancer. The fact that WATS3D accurately differentiates CD from reflux esophagitis, which is not feasible with forceps biopsy analyses, adds to its already compelling value proposition and advances our ability to achieve our vision of preventing unnecessary cancer deaths.”