Osteoarthritis is a disabling disease characterized by joint pain and restricted mobility, affecting especially the elderly. The disease generally progresses slowly, even over decades. Post-traumatic osteoarthritis, however, affects people of all ages and is initiated by joint trauma, for example, as a result of falling. The disease is most prevalent in articulating joints, such as the knee.
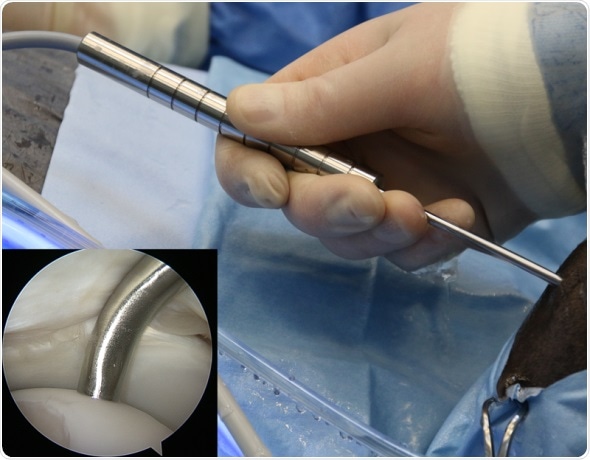
The novel arthroscopic probe in an equine knee joint in vivo with the probe tip in contact with cartilage surface (inset). Photographer: Jaakko Sarin
Although no cure currently exists for osteoarthritis, early detection of cartilage lesions could enable halting the disease progression by pharmacological or surgical means. Conventionally, joint health is diagnosed based on patients' symptoms, joint mobility and, if required, with x-ray and magnetic resonance imaging. Based on these examinations, joint repair surgery may be performed during arthroscopy. The decision on the optimal treatment option is made during the surgery, in which the joint health is evaluated visually and by palpating the cartilage surface with a metallic hook. These techniques are subjective and dependent on surgeons' experience and can, therefore, influence the treatment outcome.
An arthroscopic near infrared spectroscopic probe for evaluation of articular cartilage and subchondral bone structure and composition was developed as part of a PhD thesis at the University of Eastern Finland. The probe enables enhanced detection of cartilage injuries, as well as evaluation of the integrity of the surrounding tissue. The availability of comprehensive information on the health of joint tissues could substantially enhance the treatment outcome of arthroscopic intervention.
Previously, the near infrared spectroscopy technique has been utilized in, for example, evaluation of grain quality, but its clinical applications are still rare. However, clinical application of the technique is now possible thanks to better availability of computational power along with state-of-the-art mathematical modeling methods, such as neural networks. With these methods, the relationship between the absorption of near infrared light and tissue properties can be determined. This enables reliable determination of articular cartilage stiffness and subchondral bone mineral density — changes in these tissue properties are prognostic indicators of osteoarthritis.
Since near infrared spectroscopy is not optimal for imaging of tissues, arthroscopically applicable imaging techniques, such as optical coherence tomography and ultrasound imaging, were also used in the study. These techniques have been previously applied in intravascular imaging via specialized 1 mm diameter catheters, which are therefore well-suited for imaging narrow joint cavities. The study compared the reliability of these techniques for evaluation of chondral injuries with that of conventional arthroscopic evaluation.
Optical coherence tomography was superior to conventional arthroscopy and ultrasound imaging. In contrast to conventional arthroscopic evaluation, optical coherence tomography and ultrasound imaging provide information on inner structures of cartilage and enable, for example, detection of cartilage detachment from subchondral bone."
Researcher Jaakko Sarin from the University of Eastern Finland explains.