More and more women are undergoing 3D mammograms for breast cancer screening in the US, with rates increasing from 13 percent to 43 percent between 2015 and 2017, according to a new study published in the JAMA Internal Medicine journal.
The study claims that the new technology digital breast tomosynthesis (DBT) is more effective than 2D mammograms.
 Semnic | Shutterstock
Semnic | Shutterstock
Yale University researchers carried out a longitudinal study including 9,673,583 breast cancer screening examinations performed over three years for women between the ages of 40 and 74, with the aim of identifying patterns in the regions of the US that have adopted DBT over 2D mammography.
The study discovered that in 2015 DBT was the most popular form of breast cancer screening in 4.6 percent of hospital referral regions, but by the end of 2017, DBT was the main form of screening in 41.8 percent of hospital referral regions.
Dr. Ilana Richman, lead author of the study and an assistant professor in general internal medicine at Yale School of Medicine said the increase was “substantial” in the two-year period, adding that the “technology has become really popular.”
Regular breast screening is important in trying to find cancerous growths early to improve survival rates and lessen the need for mastectomy or chemotherapy.
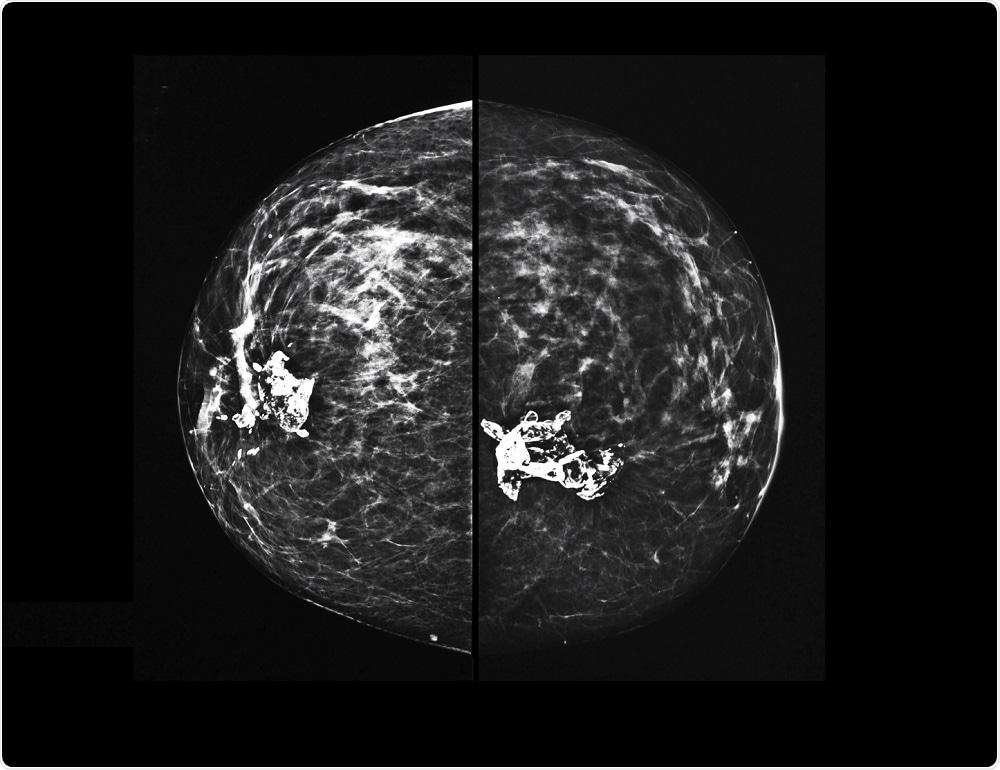
A 2D mammogram, widely used for over a decade, is an X-ray of the breasts that is able to identify cancerous growths when they are too small to see or feel. During a mammogram, each breast is compressed by a clear plate and X-ray images are taken from two angles, the front and side of the breast.
DBT, commonly known as 3D mammography, takes X-ray images of the breast from several angles and builds a 3D image of the breast. It is reported to have a lower recall rate and a better ability to detect cancer when compared with 2D mammography.
However, despite the surge in uptake of DBT, the researchers found stark differences between regions. In northeast and northwest regions of the US, the popularity of a combination of 2D and 3D mammography grew more quickly, and southeast regions showed slower increases and less uptake overall. Overall, a combination of 2D and 3D mammography was the most popular form of screening in less than 5 percent of US regions in 2015 but was the most common in 2017.
Differences in demographics taking on 3D mammography technology were also found, with regions showing high uptake of 3D mammography being predominately wealthy, white, and with higher levels of education.
The financial differences between regions and their connection to higher uptake in 3D mammography were clear. In areas with high use of 3D mammography, the average income was $53,835. In areas with the least use of 3D mammography, the average income was $45,254. Additionally, the percentage of white residents in high-uptake areas was 82.2 percent versus 70.5 percent, and a low percentage of black residents at 5.3 percent.
Robert Smith, the vice president of cancer screening for the American Cancer Society who was not involved in the study was unsurprised at these particular findings.
This is what we’ve been expecting to see for a long time. When you roll out new, higher technology and more expensive equipment, the early adopters are generally going to be in more affluent parts of the country.”
In response to the study, Dr. Joy Melnikow and Dr. Joshua Fenton said that Regional differences “could worsen existing disparities in breast cancer outcomes.”
However, as the differences in uptake between demographics were found at a population level instead of an individual level, there is no way to definitively prove that those who had higher levels of education and higher incomes were women who opted for 3D mammography over 2D.
There are advantages and disadvantages to both DBT and 2D mammography. For instance, 2D mammography can sometimes produce images suggesting cancerous growths are present when in fact the imaging has just picked up natural overlaps in tissues caused by compression needed to take the image.
In DBT, the X-ray moves in an arc over breast after it is compressed and captures images from several angles. These images are then digitized and synthesized into a 3D image of the breast.
While DBT may not be susceptible to the inaccuracies sometimes seen in 2D mammography, it uses higher doses of radiation and costs more than 2D mammograms.
Addressing the important issues of radiation dosage and cost, Smith wrote:
“The dose from these mammography exposures is very low, and therefore the true possibility that these additional exposures could cause measurable harm also is low. As for costs, it seems more and more insurance is covering 3D, so cost likely will be less of an issue over time.”
3D mammograms reduce the number of appointments needed
One “compelling” reason for patients to adopt DBT is that it reduces recall rates and lessens the amount of appointments women have to attend and importantly, the amount of radiation they are exposed to over time.
However, the radiation used by DBT is still low.
Despite this, DBT is not recommended by the US Preventative Services Task Force for routine breast screening due to insufficient evidence. For patients to get DBT, they must have it alongside 2D mammography while there are no clinical guidelines from US Food and Drug Administration (FDA) approving the imaging technique. Despite this, the American College of Radiology supports the use of 3D mammography.
Smith admits, “We don’t have enough data to say it’s definitely better […] over 2D,” and a study published in The Lancet’s Oncology journal found that DBT was “not significantly different from standard digital mammography as a screening tool for the detection of breast cancer in a population-based screening programme.”
Despite this controversy, Richman said that the study carried out by the Yale University researchers proves that the technology is “taking off” in its early phase.
Journal reference:
Hofvind, S. et al. (2019). Two-view digital breast tomosynthesis versus digital mammography in a population-based breast cancer screening programme (To-Be): a randomised, controlled trial. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(19)30161-5.