A new study hints at the possible origin of an autoimmune disease, Systemic Lupus Erythematosus (SLE).
The study, which was published in the journal Nature Immunology, shows that in SLE patients, during the early stages of B cell differentiation, signals that contribute to the expansion and activation are already present. The researchers also determined certain gene activity patterns that can be utilized as biomarkers for the disease process and progression.
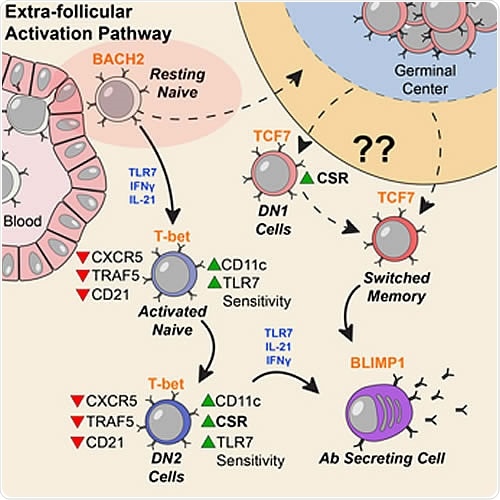
Activation can be observed at an early stage of B cell differentiation: resting naive cells (pink ellipse). Adapted from Jenks et al Immunity (2018).
The study was a result of collaboration among the two Emory laboratories of Ignacio Sanz, head of the division of rheumatology in the Department of Medicine, and recipient of the 2019 Lupus Insight Prize given by the Lupus Research Alliance, and Jeremy Boss, the chairman of microbiology and immunology. Meanwhile, Christopher Scharer, assistant professor of microbiology and immunology, co-authored the study, along with other medical experts.
Researchers analyzed the patterns of gene activity
To arrive at these results, the researchers examined blood samples from nine female patients with lupus and 12 individuals who are healthy. Initially, they classified the B cells into subgroups and determined the women’s DNA in their B-cells. During the process, the researchers analyzed the patterns of gene activity.
They also determined the DNA methylomes, transcriptomes, and chromatin accessibility profiles from five human B cell subsets from the participants. The researchers observed that patients with SLE have an increase of DN2 B cells and “activated naive”, during flare-ups or when the symptoms are severe.
Significantly, an SLE molecular signature has been established in resting naïve cells. These were also dominated by enhancement of accessible chromatin in motifs for AP-1 and Early growth response (EGR) transcription factors.
Put simply, when the researchers studied epigenetic parameters and gene activity patterns, they saw possible signs of stimulation or activation among resting naïve B cells, which occurs before the activated naive cells. Hence, the researchers note that the study could pave the way to determining when B-cells malfunction in SLE patients. The study provides vital information in understanding early antigenic triggers.
With the new discovery, the researchers hope that the study could open new paths for future research and investigation. Also, the study can help future research to determine new potential therapeutic interventions.
“Our data indicate a disease signature across all cell subsets, and importantly on mature resting B cells, suggesting that such cells may have been exposed to disease-inducing signals," the authors stated in the study.
The National Institute of General Medical Sciences and the National Institute of Allergy and Infectious Diseases supported the study.
What is Systemic Lupus Erythematosus (SLE)?
Systemic Lupus Erythematosus (SLE) is a type of autoimmune disease wherein the body’s immune system attacks its own organs and tissues. As a result, inflammation occurs in various parts of the body including the skin, heart, lungs, brain, blood cells, joints, and the kidneys.
Mainly, SLE affects connective tissues such as cartilage and the lining of blood vessels. Connective tissues provide flexibility and strength to many body structures. SLE is difficult to diagnose since the signs and symptoms are like other diseases. The common signs and symptoms vary depending on which part of the body is affected.
But, the most distinctive sign of lupus is a facial rash that looks like butterfly wings that unfold across the cheeks. Though the rash occurs in most cases, some patients may not have one.
If not detected early, it can affect many body organs. About one-third of people with SLE develop kidney diseases or nephritis. In some patients, they develop heart disease called pericarditis, the inflammation of the heart’s sac-like membrane. Others develop problems with their heart valves. Aside from these SLE can cause severe diseases affecting the nervous system, including stroke, cognitive impairment, and peripheral neuropathy. In some cases, the patients develop respiratory failure.
Journal reference:
Epigenetic programming underpins B cell dysfunction in human SLE, Christopher D. Scharer, Emily L. Blalock, Tian Mi, Benjamin G. Barwick, Scott A. Jenks, Tsuneo Deguchi, Kevin S. Cashman, Bridget E. Neary, Dillon G. Patterson, Sakeenah L. Hicks, Arezou Khosroshahi, F. Eun-Hyung Lee, Chungwen Wei, Iñaki Sanz & Jeremy M. Boss, ttps://doi.org/10.1038/s41590-019-0419-9
DO - https://www.nature.com/articles/s41590-019-0419-9