A new portable device that utilizes artificial intelligence (AI) and biosensors can rapidly detect if cancer cells thrive after chemotherapy treatment.
A team of researchers at Rutgers University has designed a new portable device that is up to 95.9 percent effective and accurate in counting living cancer cells when they pass through certain electrodes. This way, doctors can see if the targeted chemotherapy treatment was effective.
Published in the journal Microsystems & Nanoengineering, the study aims to devise a new and simple method to rapidly assess drug efficacy in targeted chemotherapy cancer therapy, where anticancer drugs are conjugated to antibodies that target surface markers on cancer cells.
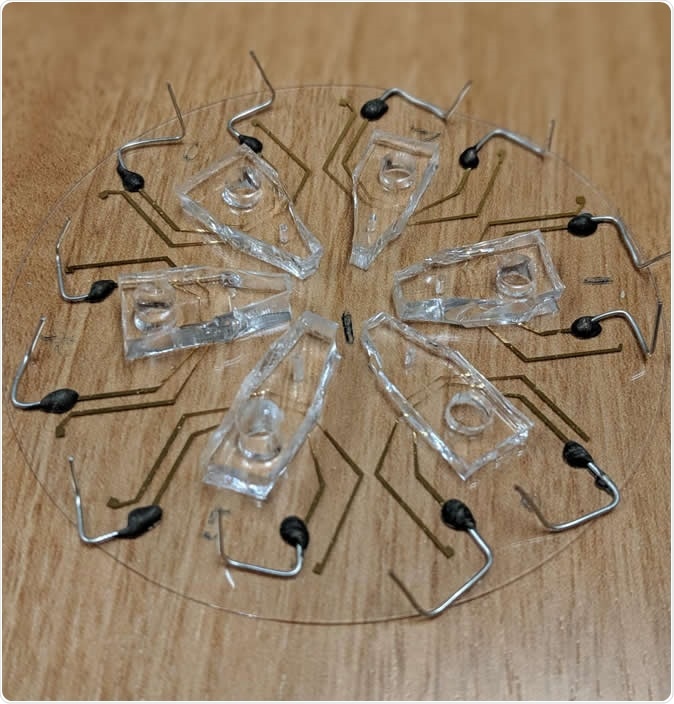
This image shows six devices with biosensors to detect whether a cancer cell is alive when it passes through a tiny hole for fluids. The devices fit on a 3-inch wide piece of glass. Image Credit: Zhongtian Lin
Targeted cancer treatment
Cancer continues to be one of the leading causes of mortality and death across the globe. The major treatment options for cancer are surgery, radiation therapy, chemotherapy, hormonal therapy, targeted therapy, and palliative care.
The treatment of cancer often involves using drugs to kill the tumor cells. However, chemotherapy kills both cancer cells and healthy cells, causing several side effects such as serious gastrointestinal problems and hair loss.
On the other hand, a targeted chemotherapy approach uses anti-cancer drugs but only tumor cells are killed. The approach causes minimal effects on healthy cells, leading to higher efficacy and lesser side effects.
It’s important to develop new agents and diagnostic tools to predict patient response on targeted therapy.
Novel device to detect living cancer cells after treatment
After a targeted therapy, there isn’t an effective way to determine if all cancer cells were eradicated. Now, the team built a portable platform that can predict if patients will effectively respond to targeted chemotherapy treatment.
To build the device, they used AI and state-of-the-art biosensors, to analyze small amounts of fluids to detect if cancer cells are either responsive or resistant to certain chemotherapy drugs.
The device can provide immediate results, prompting for individualized patient treatments and at the same time, improved detection and management of cancer. With its features, it rapidly checks cells without having to stain them, permitting enhanced molecular analysis and immediate results.
At present, there are devices that can detect thriving cancer cells after treatment, but they depend on straining the cells.
To test the device, they used cancer cell samples treated with various targeted anticancer medicine concentrations. The device was able to detect whether there is a living cancer cell based on the shift in its electrical properties as it passes through a small fluidic hole.
The researchers plan to test the device on tumor samples from patients and hopefully, the device can be utilized to test cancer therapies on patient tumor samples, before any treatment is initiated.
In this work we built a device capable of rapidly analyzing cell viability without staining of cells, which allows for further downstream molecular analysis,” the authors concluded.
“Compared to optical techniques for label-free analysis of cell viability, our novel method can rapidly analyze cell viability with minimal cost. We envision using this device as a point-of-care diagnostic for assessing patient response and personalization of therapeutics,” they added.
The team of researchers, headed by Joseph Bertino, a professor at Rutgers Robert Wood Johnson Medical School and a resident researcher at Rutgers Cancer Institute of New Jersey, formerly developed a treatment option that can target cancer cells, like multiple myeloma, epithelial carcinomas, and B-cell lymphoma.
The approach uses a chemotherapy drug that binds to an antibody so only tumor cells are detected and targeted. This helps minimize interaction with non-cancer or healthy cells, reducing the occurrence of serious side effects.
"Novel technologies like this can really have a positive impact on the standard-of-care and result in cost-savings for both healthcare providers and patients," Bertino explained.
Cancer by the numbers
Every year, the American Cancer Society estimates the number of new cancer cases and deaths in the United States. They found that 1,762,450 new cancer cases and 606,880 cancer deaths are estimated to occur in the country in 2019. Overall, the cancer death rate decreased between 1991 and 2016 by as much as 27 percent. In 2012, there were 14.1 million new cases and 8.2 million cancer-related deaths across the globe.
The most common forms of cancer are breast cancer, lung and bronchus cancer, colon or rectum cancer, prostate cancer, bladder cancer, melanoma (skin cancer), renal pelvis cancer, non-Hodgkin lymphoma, kidney cancer, leukemia, pancreatic cancer, thyroid cancer, liver cancer, and endometrial cancer.
Journal reference:
Toward point-of-care assessment of patient response: a portable tool for rapidly assessing cancer drug efficacy using multifrequency impedance cytometry and supervised machine learning, Karan Ahuja, Gulam M. Rather, Zhongtian Lin, Jianye Sui, Pengfei Xie, Tuan Le, Joseph R. Bertino & Mehdi Javanmard, Microsystems & Nanoengineeringvolume 5, Article number: 34 (2019), DOI: 10.1038/s41378-019-0073-2, https://www.nature.com/articles/s41378-019-0073-2