Osteoarthritis (OA), also called degenerative joint disease, is the most common chronic condition of the joints. Since the disease is degenerative, it is the single most common cause of disability among older adults, with about 10 to 15 percent of all adults who are more than 60 years old have some degree of osteoarthritis, with more women affected than men.
Currently, osteoarthritis is treated with lifestyle changes, exercise, therapies, and medications, including steroid injections. However, a new study by researchers at Boston University School of Medicine found that steroid injections in the hips and knees of patients with osteoarthritis are more dangerous than previously thought.
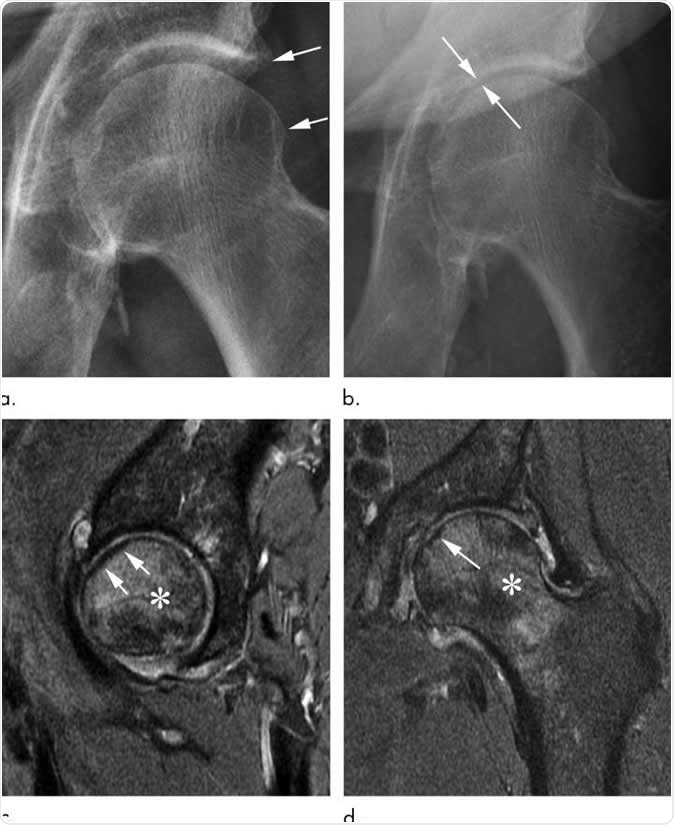
Rapid progressive osteoarthritis joint space loss (type 1) and subchondral insufficiency fracture in a 53-year-old man who presented with hip pain. (a) Anteroposterior left hip radiograph shows mild osteophytic changes (arrows) and no joint space loss. This patient was referred for intra-articular corticosteroid injection. (b) Seven weeks after injection, he returned with worsening hip pain. Repeat anteroposterior left hip radiograph shows accelerated loss of joint space (arrows). (c) Sagittal intermediate-weighted fat-suppressed MRI obtained at the same time as b shows a linear subchondral hypointensity representing subchondral insufficiency fracture of the anterior superior femoral head with subtle flattening of the overlying articular surface (arrows). Extensive bone marrow edema extends to the femoral neck. (d) Corresponding coronal intermediate-weighted fat-suppressed MRI enables us to confirm the presence of a subchondral insufficiency fracture (arrow) and depicts the true extent of bone marrow edema. Image Credit: Radiological Society of North America
Potential risks of steroid injections into joints
They discovered that accelerated arthritis and joint damage could be one complication and unintended result of corticosteroid injections.
Steroid injections may lead to joint collapse and may speed up the need for total hip or knee replacement. Usually, corticosteroids are used to stem inflammation in arthritis, and they’re usually injected into the joints to relieve pain and swelling.
The study, which was published in the journal Radiology, reveals how corticosteroids, though it can relieve pain and inflammation, is tied to complications that can potentially hasten the destruction of the joint.
“We are now seeing these injections can be very harmful to the joints with serious complications such as osteonecrosis, subchondral insufficiency fracture and rapid progressive osteoarthritis," Dr. Ali Guermazi, chief of radiology at VA Boston Healthcare System and professor of radiology at BUSM, said.
"Intra-articular corticosteroid injection should be seriously discussed for pros and cons. Critical considerations about the complications should be part of the patient consent, which is currently not the case right now," he added.
The study authors reviewed existing literature on the complications of steroid injections. They have determined four main adverse effects of the treatment, namely rapid joint destruction with bone loss, complications from osteonecrosis or bone tissue death, subchondral insufficiency fractures like stress fractures, and accelerated osteoarthritis progression with loss of the joint space.
What doctors can do
The researchers recommend that when physicians prescribe steroid injections, there should be consent forms that include injection-associated risks. The consent should include that the injection may lead to rapid progressive osteoarthritis and joint collapse. This way, patients are aware of the risks involved in the treatment.
They also suggest that the radiologic community should participate in research on the topic. This way, they can improve practice and understand the potential at-risk conditions before the patient receives treatment.
Moreover, physicians should carefully inspect and examine patients with mild or no osteoarthritis on radiology results, who were referred to receive these injections. The physician should also consider telling younger patients of potential risks of the injections, and should opt for other therapies and lifestyle changes first.
“Physicians do not commonly tell patients about the possibility of joint collapse or subchondral insufficiency fractures that may lead to earlier total hip or knee replacement. This information should be part of the consent when you inject patients with intra-articular corticosteroids,” Dr. Guermazi said.
What is osteoarthritis?
Osteoarthritis (OA) is the most common form of arthritis, and it’s more common in women than in men. It is one of the most frequent causes of physical disability among seniors.
The condition happens when the cartilage, which works by providing cushion at the ends of the bones in the joints, wears away and breaks down. As a result, the bones rub against each other, causing severe pain and swelling.
The most common signs and symptoms of osteoarthritis include pain, decreased range of motion, decreased flexibility, swelling, and stiffness. The common risk factors include obesity, old age, and family history.
Treatment of osteoarthritis focuses on increasing physical activity, muscle strengthening exercises, taking pain killers and anti-inflammatory medicines, supportive devices, and surgery.
In the United States, about 30 million adults are living with osteoarthritis.
Journal reference:
Kompel, A., Roemer, F., Murakami, A., Diaz, L., Crema, M., and Guermazi, A. (2019). Intra-articular Corticosteroid Injections in the Hip and Knee: Perhaps Not as Safe as We Thought? Radiology. https://pubs.rsna.org/doi/10.1148/radiol.2019190341