This bionic pacemaker follows the natural change in heart rhythm that occurs with breathing, and causes a steep improvement in the efficiency at which the heart supplies blood to the body. The disappearance of this physiological phenomenon in a diseased heart is a predictor of a poor outcome and of sudden death due to a cardiac cause.
Why pacemakers are used
Heart failure affects about 26 million people all over the world, with about 6 million adults in the US and 900 000 people in the UK suffering from this chronic and often crippling condition. The mortality in this illness is about 50% at 5 years from diagnosis. Besides immense health costs and the high death rate, life can be extremely burdensome for such patients. Many of them are fitted with cardiac pacemakers to keep the struggling heart beating at a regular rate, so as to optimize the work it does at the least possible effort.
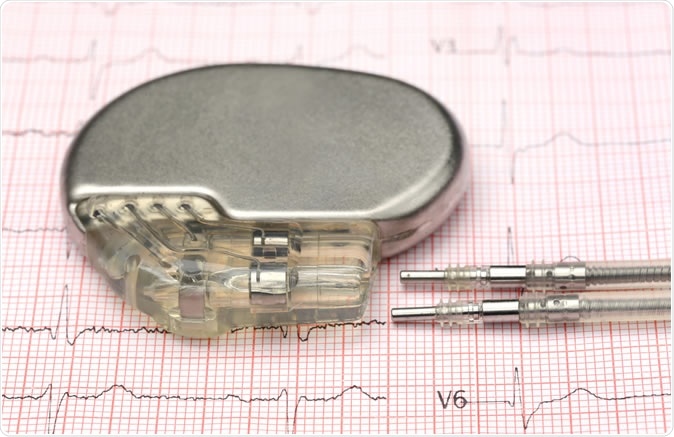
Close up of pacemaker on electrocardiograph. Image Credit: Swapan Photography / Shutterstock
Cardiac pacemakers are also often used to treat patients who have survived a heart attack. About 1.4 million such survivors live in the UK alone. In the US, there are over a million heart attacks or angina episodes each year. About 86% of these patients survive, while a third may expect to have a recurrence in the future. Pacemakers are used in those who have had a heart attack for several indications. The heart muscle may have been injured badly, and requires an externally generated rhythm because it beats too slowly. Sometimes the nerve pathways that conduct the electrical impulse from the natural pacemaker region are damaged and fail to carry it all over the heart as usual, leading to irregular and uncoordinated contraction. This can quickly lead to heart failure and death.
Heart failure is not a curable condition, but its progress can be slowed considerably by taking medication to strengthen heart contraction, enhance blood vessel function, and prevent fluid buildup in the lungs.
Conventional and bionic pacemakers
The normal heartbeat is a dynamic phenomenon. With every intake of breath, it can be felt to speed up, only to slow down with exhalation – a fascinating change in speed and rhythm called respiratory sinus arrhythmia. There are also several more minor other body processes which modulate the heart rate, causing normal heart rate variability. This became the basis for a new type of pacemaker called a respiratory modulated heart rate pacemaker, which adapts the rate of impulse generation to the breathing, because this allows more blood to be pushed out when more blood is received by the heart during inhalation, and less when the heart is being pushed in by the chest collapse that accompanies exhalation.
Most automatic pacemakers generate a metronome-like rhythm when the patient is at rest, irrespective of the body’s other operations. This doesn’t take advantage of the natural changes that occur in the body. The researchers took note of the poorer prognosis linked to the lack of the natural respiratory sinus arrhythmia to design a new model that would follow this waxing and waning rhythm, and hopefully improve the performance of the heart.
Study findings
To test the new pacemaker the researchers used exquisitely precise echocardiography signals to look at how the heart is pumping before and after pacing for two weeks, in rats that had been induced to develop heart failure. They monitored these heart failure rats with conventional pacemakers as well as the new model, over a period of 2 weeks. They also had a control group of unpaced rats with heart failure.
Researcher O’Callaghan reports, “Within two weeks there was a 20 per cent increase in blood pumped by the heart which was not the case when we used conventional pacemakers.” The cardiac output as well as the stroke volume shot up in the rats who had a pacemaker set to respiratory sinus arrhythmia, compared to those using the other monotonic pacing.
Cardiac output refers to the total volume of blood pumped out from the heart in one minute. The stroke volume refers to the amount of blood pumped from the left ventricle in a single contraction.
The RMH rats also had better ventricular muscle contractility and improved blood flow through the coronary arteries. The mechanism of this improvement was stronger heart muscle contraction, which continued to manifest even after the period of treatment with the pacemaker. This led to the suggestion that the RMH pacing actually reverses undesirable changes in the anatomy of the heart.
Implications
Clinical cardiologists like the Bristol Heart Institute’s Ed Duncan share the researchers’ excitement, commenting, “This approach may represent a novel therapy in addition to those already available for the treatment of heart failure.”
Indeed, the pacemaker may represent a big step forward in designing physiologic pacemakers that can ease the heart’s burden while improving its performance, and thus making life more bearable for patients with cardiac failure. The scientists suggest that providing this more natural form of pacing improves the way the heart functions after an injury by reversing harmful changes in the heart muscle thickness and heart size. This process, called reverse remodeling, not only serves as an estimate of treatment effectiveness but predicts patient outcome.
The researchers now plan to take the design forward into a clinical trial phase in humans, to see if the same outcomes occur when respiratory sinus arrhythmia is used to guide pacemaker stimulation of the heart contractions.
Journal reference:
Enhancing respiratory sinus arrhythmia increases cardiac output in rats with left ventricular dysfunction. Erin L. O'Callaghan, Renata M. Lataro, Eva L. Roloff, Ashok S. Chauhan, Helio C. Salgado, Edward Duncan, Alain Nogaret, and Julian F. R. Paton. Journal of Physiology, 2019. https://doi.org/10.1113/JP277293. https://physoc.onlinelibrary.wiley.com/doi/10.1113/JP277293