A new study being presented at the yearly conference of the Radiological Society of North America (RSNA) reports that MRI scanning of the brain shows signs of brain damage in obese adolescents – and that these signs could be the result of brain inflammation.
The US is witnessing an unprecedented rise in obesity, both in young and old. Adolescent obesity has all the potential to become a huge public health problem. The percentage of obese individuals in childhood and adolescent having already increased by over 300% in the last fifty years, according to the statistics issued by the Centers for Disease Control and Prevention. The World Health Organization (WHO) reports that globally, obesity in infancy and young children below the age of 5 has gone up from about 32 million a year to about 41 million, between 1990 and 2016.
Obesity is linked to weight gain, abnormal blood sugar control, high blood lipid levels, hardening of the arteries, osteoarthritis and infertility, among a host of other medical conditions. However, the current study raises concern about the role of obesity in provoking inflammation within the nervous system that in turn results in damage to certain vital areas of the brain.
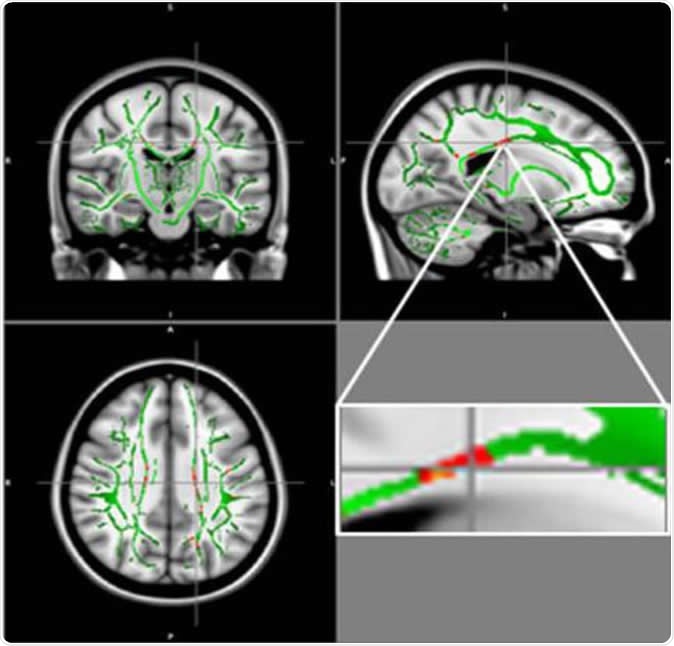
Reduction in fractional anisotropy (FA) in obese patients compared to the control group: At the intersection of the alignment vectors, a large cluster of FA decrease located in the corpus callosum on the left. In red: Reduction of FA in obese patients compared to controls, and FA skeleton (green), superimposed on the mean of FA images in sample.
The study
Magnetic resonance imaging (MRI) is a flexible and powerful tool for imaging the central nervous system. Contrast is often produced by measuring the degree to which the signal weakens due to the diffusion of water. In the current study, the researchers used an MRI method called diffusion tensor imaging (DTI) in which the passage of water by diffusion along the white matter bundles of the brain can be traced to outline these pathways. These bundles, or tracts, are important because they transmit nerve impulses, being composed of nerve fibers for the most part. Using DTI, direct evidence of damage can be picked up because this technique reflects microstructural and architectural changes in the brain matter.
Water diffuses inside, outside, around and through cell-based structures, and this movement is affected by the presence of cell membranes and organelles. For instance, a cell membrane forces the water to move more circuitously, reducing the displacement. In white matter, the diffusion occurs quite freely in a direction parallel to the orientation of the nerve fibers, but very little in a perpendicular direction. This is called anisotropic diffusion. It is described by an equation which yields a quantity called the diffusion tensor. This serves as a sensitive probe to sense normal and abnormal microstructure of tissue.
The researchers performed DTI in about 60 healthy and 60 obese teenagers, between the ages of 12 and 16 years. They used the results to calculate a measure called fractional anisotropy (FA) that corresponds to the state of health of the white matter of the brain. The lower the FA value, the greater the damage in the white matter.
Pamela Bertolazzi - Brain changes on obese child/ Alterações cerebrais na obesidade infantil - CAISM
The findings
The study showed low FA values in obese teenagers in the area of the brain called the corpus callosum. This is the large bundle of white matter that links the two brain hemispheres and helps to coordinate all brain activity. Another area that showed low FA measurements was in the middle orbitofrontal gyrus, which is linked to emotional control and to reward pathways. These have been linked to addiction patterns of behaviour.
Moreover, the researchers found that not a single area in the brain of obese adolescents showed increased FA. The authors relate these brain changes to damage in important brain regions that regulate the appetite, thinking and emotions.
The damage occurs in a pattern that corresponds, at least in part, with leptins. Leptins are molecules that act as hormones to control energy levels and fat stores in the body. This also acts as a marker of inflammation. In some obese individuals at least, leptin loses its ability to regulate brain areas linked to appetite and food intake. As a result, the person keeps on eating despite the presence of fat stores that are more than adequate. Leptin resistance has set in, leading to the overproduction of leptin.
White matter damage is also linked to high insulin levels. Insulin is a hormone produced by the pancreatic gland, tucked away behind the stomach, that regulates blood sugar levels. Insulin resistance is a common phenomenon in obese people and is linked to multiple metabolic dysfunctional states.
Implications
In the current study, the brain maps showed that brain changes were linked to leptin and insulin markers. Inflammatory markers were also increased in such damaged areas. The researchers say this suggests that neuroinflammation is at work in addition to the body’s resistance to insulin and leptin.
More studies will be needed to confirm that brain inflammation in young obese individuals is indeed due to brain structural damage. The scientists plan to repeat the MRI scans in the same population after they have been treated for obesity, by a multidisciplinary approach. This will show if the damage can be reversed by weight loss.
Source:
Decrease of White Matter Integrity in Obese Adolescents: Study of Diffusion Tensor Imaging (DTI) - https://press.rsna.org/pressrelease/2019_resources/2121/abstract.pdf