Gut diseases are difficult to diagnose in many cases, and their underlying dysfunction is hard to understand in many cases. Now, a new study published in the journal Molecular Omics promises to uncover a better insight into how these conditions occur and their mechanisms, by providing a deeper look at how genes interact in complex ways in health and fail to do so in disease. This is by an original network of computational and experimental processes designed to point out the master regulator genes of the gut, and those involved in the pathogenesis or maintenance of inflammatory bowel disease (IBD).
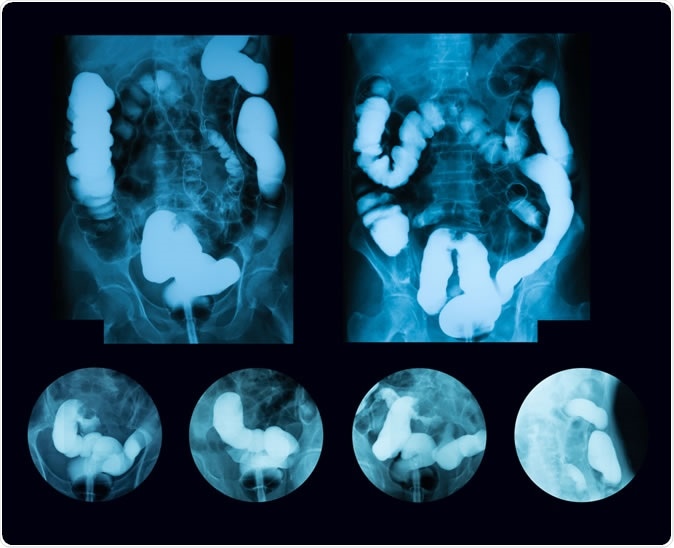
Barium enema double contrast, case of sigmoid colon cancer (Inflammatory Bowel Disease: IBD). Image Credit: Suttha Burawonk / Shutterstock
Gut cells
The gut contains a whole array of distinctive cells each with multiple functions and roles. For instance, Paneth cells secrete specialized peptides, short strings of amino acids, that act to protect the gut against microbial infection. Goblet cells release mucus, a thick protective glairy layer that keeps acid, digestive juices and bacterial products safely out of contact with the surface epithelium of the digestive tract. When these cells fail to perform their function normally, IBD and other disease conditions can set in.
Organoids
Organoids are stem cells cultured to form small 3-dimensional masses of human epithelial cells. The cells are taken either from patients or from experimental mice. The aim is to create a small-scale model of the human gut and how it reacts to various therapies. This is one way to research and bring about precision medicine.
In the current study, the researchers looked at enteroids – the organoids produced from small intestinal epithelium. Modifying these organoids by, for instance, enriching it with more cells of one kind (encouraging the differentiation of more cells of a particular type), can also help understand how important different cell types are inside the whole system. It also allows research into how various genes interact in health or disease. The million-dollar question is, is such modification consistent with the modeling function of the system or does it destroy its role as a model?
The current study aimed to help answer this query. The researchers set up a linear sequence of analytical tasks that generates a profile of the mRNA, microRNA and long noncoding RNA expressed in these organoids to help achieve a direct comparison of gene expression in organoids enriched for one of these cell types, and in those that are not. These datasets are then compared to another database that includes all the gene interactions currently known – which is growing all the time. For instance, using a network approach, they predicted that if more Paneth cells were present, key regulatory molecules like Cebpa, Jun, Nr1d1 and Rxra which specifically modulate Paneth cell function will be expressed at higher levels. Similarly, they predicted regulatory molecules for goblet cells and for others when both were expressed.
Researcher Agatha Treveil says, “Based on our transcriptomics analysis, we see clear increases in targeted cell types as we expected from using the organoid enrichment methods.” This is a far superior method to sequencing the transcriptomes of single cells within tissue samples to find out how many of each type of epithelial cell type is found in the intestines of healthy people and patients with IBD. They also found that when more of one type of cell is preferentially differentiated, enteroendocrine cells are also enriched.
Implications
This work means that regulatory genes can now be tagged, and in particular those that are involved in controlling multiple processes and are thus essential for the normal functioning of Paneth and goblet cells.
The researchers discovered that among these genes, many showed an overlap with genes involved in inflammatory reactions and in IBD. Either before or after Paneth/goblet cells differentiate, the regulatory environment is rewritten, and this could partially explain the onset of IBD. This not only confirms the major part played by Paneth cells in IBD but also shows an alternative mechanism to explore this subset of gut illnesses.
Some limitations exist, such as the inhibitory effect of certain molecules used to enrich a particular cell type on other cellular pathways.
Calling this a “pioneering step forward in establishing a pipeline to better understand the gene networks at play in the gut,” Treveil goes on to say that this work will help them set up new experiments to explore related processes in a deeper way. The all-in-one systems biology setup will be useful not only to examine the organoids built up from stem cells retrieved from patients with IBD, according to researcher Tamas Korcsmaros, but will allow them to analyze the effects of a probiotic or a drug on any important cell type in the gut.
Journal reference:
Regulatory network analysis of Paneth cell and goblet cell enriched gut organoids using transcriptomics approaches. A. Treveil, P. Sudhakar, Z. J. Matthews, T. Wrzesiński, E. J. Jones, J. Brooks, M. Ölbei, I. Hautefort, L. J. Hall, S. R. Carding, U. Mayer, P. P. Powell, T. Wileman, F. Di Palma, W. Haerty and T. Korcsmáros. Molecular Omics. https://pubs.rsc.org/en/content/articlelanding/2020/MO/C9MO00130A#!divAbstract