The use of mathematical modeling in the study of biological systems has become a challenging and rewarding field of research as it yields many unknown pieces of information. A new study published online on December 16, 2019, in the journal Proceedings of the National Academy of Science (PNAS).
The combination of RNA sequencing with bioinformatics to inform a new mathematical model has now come up with a novel way to predict the occurrence of liver cancer. It is called the tumorigenic index score, and it describes the sudden occurrence of a switch in the way the RNA decodes the DNA blueprint, that causes liver cells to develop in a cancer cell pathway rather than a healthy one.
UC San Diego School of Medicine researchers developed a mathematical equation to predict when healthy liver cells become cancerous before tumors are visible in a standard clinical setting.
Liver cancer
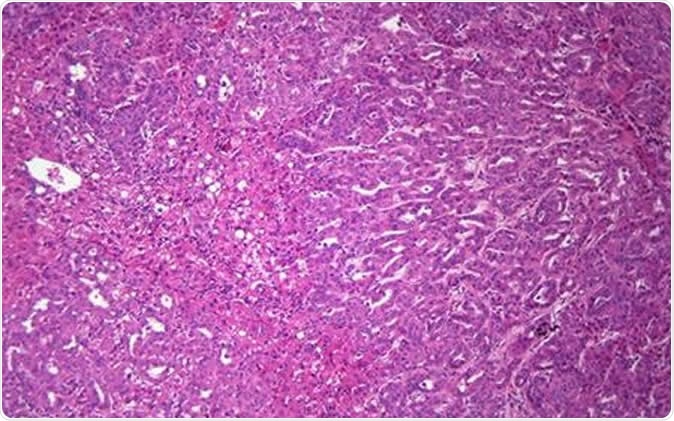
Liver cancer is a malignant tumor that starts within one or more of the various cells that make up the liver. Most commonly it is a hepatocellular carcinoma, which begins in the basic liver cell or hepatocyte. However, there are also intrahepatic cholangiocarcinomas and hepatoblastomas which arise from other types of cell found in the liver.
About 700,000 cases of liver cancer are diagnosed every year and 600,000 people die of this disease over the same period. It is estimated that within the US, 42,000 new cases and 31,000 deaths will occur over the year 2019.
The clinical features of liver cancer occur only in the later stages of the disease. They include:
- Losing weight unintentionally
- Jaundice
- Loss of appetite
- Nausea and vomiting
- Weakness and tiredness without obvious cause
- Pale bulky stools
Liver cancer causes
Like other cancers, liver cancer is the result of a mutation in the DNA that drives the cell to proliferate in an uncontrolled manner and to spread deeper, wider and to distant locations. The specific cause of the mutation is often unknown, though in some cases, such as cervical and oropharyngeal cancer, infection with certain strains of the human papilloma virus (HPV) is implicated.
Similarly, chronic infection with hepatitis B, hepatitis C, alcoholic and non-alcoholic cirrhosis, toxins in certain grains and nuts produced by molds growing on them because of poor storage conditions, non-alcoholic fatty liver disease, diabetes and certain inherited liver diseases are known to increase the risk of liver cancer.
The need
Liver cancer is currently not treatable by chemotherapy once it has advanced too far to be completely resectable. Hence, late liver cancer is essentially an incurable condition. Considering that the tumor should not exceed 1 cm in diameter if it is to be treated early, this gives a very short window of opportunity.
Researcher Gen-Sheng Feng says, “Early detection of liver cancer, when a tumor is less than 10 millimeters, allows oncologists to better treat, surgically remove and kill cancer cells. For the first time, we have a mathematical equation that can predict when healthy liver cells become cancerous and, importantly, we are able to detect cancer cells before tumors are visible in a standard clinical setting.”
The study
The scientists developed an analytical tool that examines clustered transcription factors, the proteins that actually drive the decoding of DNA segments (genes) to form RNA. RNA is the messenger molecule that directs the cell to produce the corresponding proteins from the transcribed gene. Transcription factors bind to the gene at various regions called the promoter, enhancer, and inhibitor, for instance, to direct the gene to turn off or on within the cell at any given time. The scientists measured the amount of the transcription factors being expressed along with the target genes that they influence, with these two types of molecules forming a transcription factor cluster.
The team then analyzed the RNA sequencing data from cells in the precancerous and cancerous stages of the liver in experimental mice in which various liver cancers were induced, as well as other chronic liver conditions like steatosis, cirrhosis and fibrosis.
The results – the transcriptome switch
The analysis showed that there were significant changes in the level of expression of 61 transcription factor clusters in mice that had cancer. Some were upregulated, or expressed at a higher level, while others were downregulated, or expressed less. Some of the transcription factors involved were identified for the first time as being linked with liver cancer.
They then used this data to create a complete analysis of the complete RNA sequence set in a single liver cell – the transcriptome. Repeating the process on a large number of cells, they were finally in a position to compare how transcription factor clusters looked like in a healthy liver and in a liver affected by chronic liver disease. In the latter, they analyzed these clusters at various stages of the disease. By refining their analysis in this way, they were finally able to pinpoint the stage at which accumulated tumorigenic signals abruptly switch the cell metabolism to that of a liver cancer cell instead of a healthy cell.
Using this data, they further developed a method by which they could calculate the tumorigenic index (TI), based on the measurement of the strength with which tumorigenic signals were being produced in the transcriptome, and especially in the transcription factor clusters.
Study in humans
So far, all the data applied to the model had been taken from mice. Now the researchers switched to human data, which they retrieved from a public database of human medical records. They used the same analytical tool to go through this data. Gratifyingly, they correctly identified patients who had cancer, those who had chronic liver disease, and in a subset of patients with cirrhosis, who have a higher risk of developing cancer, they identified those who were likely to develop it by using their tumor index score. In some patients, they identified the presence of tumor nodules so small as to have been imperceptible by clinical examination.
Once the tool has been tested rigorously and on a wider scale, it will be ready to use on liver biopsies, to predict whether liver cancer is present in these specimens. Finally, Feng hopes, they will be able to predict the risk of this condition and to assign a stage for it if present, using blood samples.
The researchers are optimistic about the future value of their tool. Says Feng, “This mathematical approach can be developed into a risk assessment and early diagnostic tool of liver cancer development for a larger population of people living with chronic liver disease, particularly those with cirrhosis.” Not only will this be important in treating patients with precision medicine, but the same principle can be used to predict more cancers as well.
Source:
Journal reference:
A tumorigenic index for quantitative analysis of liver cancer initiation and progression Gaowei Wang, Xiaolin Luo, Yan Liang, Kota Kaneko, Hairi Li, Xiang-Dong Fu, Gen-Sheng Feng Proceedings of the National Academy of Sciences Dec 2019, 201911193; DOI: 10.1073/pnas.1911193116, https://www.pnas.org/content/early/2019/12/10/1911193116