Menopause marks the end of a woman’s reproductive years, which normally occurs in their 50s. The time at which a woman undergoes menopause may indicate future health status, with those having premature menopause at a higher risk of developing multiple and chronic health problems, a new study found.

Image Credit: fizkes / Shutterstock
After menopause, it’s expected for women to experience body changes linked to fluctuating hormonal levels. In past studies, it was known that reduced levels of estrogen have been associated with a higher risk of developing cardiovascular disease, breast cancer, and hypertension, among others.
A team of researchers at the Center for Longitudinal and Life Course Research at The University of Queensland, Brisbane (Australia) has found that women who experience early menopause or premature menopause are almost three times more likely to develop medical problems in their 60s, compared to those who had their menopause at the age of 50 or 51.
The study, published in the journal Human Reproduction, highlights how premature menopause affect a woman’s health. Women with premature menopause experience heightened odds of developing chronic conditions and multimorbidity. Natural menopause is defined as a stage when a woman has no monthly period for 12 months.
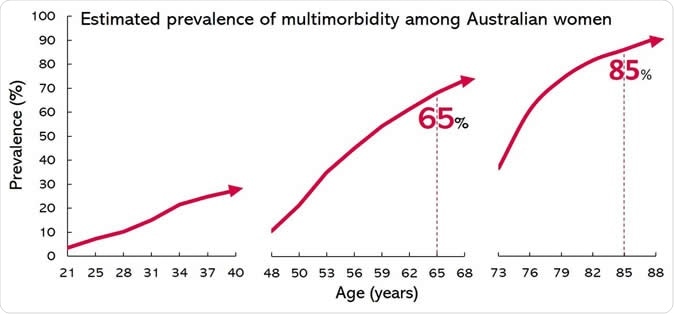
Estimated prevalence of multimorbidity among Australian women. Image Credit: Human Reproduction
Multimorbidity and premature death
The data were drawn from 5,107 women in an Australian national health survey known as the Australian Longitudinal Study on Women’s Health between 1946 and 1951. The women had the first survey in 1996 and answered the succeeding ones every three years until 2016.
In the survey, the women were asked if they had been diagnosed or treated with 11 health problems, including high blood pressure, diabetes, heart disease, arthritis, stroke, asthma, osteoporosis, depression, chronic obstructive pulmonary disease, anxiety, and breast cancer.
In the 20th year of follow-up, 2.3 percent of women experienced premature menopause, and 55 percent developed multimorbidity, which means that women have two or more of these health conditions. About 71 percent of the women with premature menopause developed two or more of the health problems by the age of 60 compared to just 55 percent in those with a normal menopause onset.
Further, they found that 45 percent of women with premature menopause had developed multimorbidity in their 60s, compared to those who had menopause at the age of 50 to 51 years old. Those with premature menopause also experienced a higher incidence of most individual chronic conditions.
“Our findings indicate that multimorbidity is common in mid-aged and early-elderly women. Premature menopause is associated with an increased risk of developing multimorbidity, even after adjusting for previous chronic conditions and for possible factors that could affect the results, such as whether or not the women had children, how many, education, body mass index, smoking, and physical activity,” Professor Gita Mishra, director of the Centre, said.
Body changes during menopause
Every woman will experience menopause one way or another, at different times. In some women, it may happen earlier than the others. During menopause, women may have many body changes mainly due to hormone levels of estrogen.
When a woman grows old, the ovaries age and may reduce the number of hormones it releases. When this happens, the hormones and organs won’t work the same way. Estrogen, for instance, decreases and it can cause many body changes and can negatively impact health.
Lower estrogen levels are tied to many health issues, including infertility, irregular periods, weak bones, hot flashes, depression, increased risk of urinary tract infections, and painful intercourse.
It’s also linked to a higher risk of developing health conditions such as cardiovascular risk, high blood pressure, obesity, and osteoporosis.
Journal reference:
Xiaolin Xu, Mark Jones, Gita D Mishra, Age at natural menopause and development of chronic conditions and multimorbidity: results from an Australian prospective cohort, Human Reproduction, , dez259, https://doi.org/10.1093/humrep/dez259