Drug resistance is among the greatest threats to worldwide health. If bacterial infections could be sensed early enough to treat them before they take a hold on the patient, it would help avoid serious infections. And if the bacteria resist the antibiotic, being able to detect this would be crucial in switching drugs to arrest the infection before it spreads.
At present, the methods of detecting antibiotic resistance are expensive, require professional expertise, and take too much time. Moreover, using antibiotics for infections that are resistant to them promotes even more drug resistance.
Colorimetric methods to the rescue
The new study describes a way of doing just this, based on a color-changing material. Described as “a portable paper-based band-aid (PBA)”, it is a colorimetric way of sensing and treating sensitive bacterial infections while signaling the presence of drug-resistant bacteria as well.
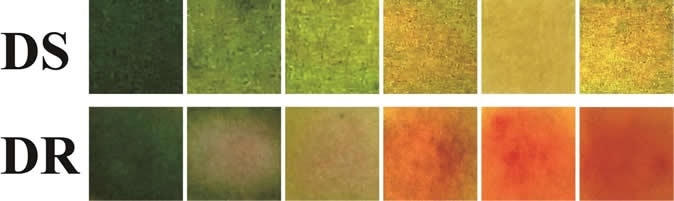
A bandage changed color from green to yellow, and from green to red, in the presence of increasing concentrations of drug-sensitive (DS) and drug-resistant (DR) E.coli, respectively. Image Credit: Adapted from ACS Central Science 2020, DOI: 10.1021/acscentsci.9b01104
Early detection of infection in this study exploits the microenvironment of bacterial growth, which includes an acidic pH, various toxins and enzymes. Acidity is an easy way to track the presence of pathogenic bacteria because it is due to their breakdown of glucose. Drug resistance, on the other hand, depends on the presence of the beta-lactamase and similar enzymes. The presence of beta-lactamase is a widely used indicator of bacterial antibiotic resistance because it denotes resistance to the extremely common beta-lactam antibiotics.
Once drug resistance has been identified, photodynamic therapy and other similar treatments have been adopted to increase the level of reactive oxygen species (ROS). These molecules act on multiple cell targets associated with drug resistance, including the bacterial cell wall, nucleic acids, and proteins. A careful use of this strategy is necessary since ROS attack healthy cells and bacteria indiscriminately.
The innovation
The need of the hour is a portable, cheap and accurate device to detect and overcome antibiotic resistance. Paper-based platforms, including biosensors and sterilization paper, have stolen the limelight in this regard because of multiple advantages: low cost, sustainability, safety, and ease of adjustment. The current study focuses on a paper-based bandage device to detect and treat infection selectively after sensing antibiotic resistance.
The basis of the bandage is colorimetry. It contains bromyothymol B that is green at first but becomes yellow on encountering acids that are found in the microenvironment of a bacterial infection. In this situation, the material releases an antibiotic, ampicillin, loaded on nanoparticles and coated with the sugar chitosan that attracts bacteria due to their negative charge. When the nanoparticles come into contact with the acid environment, they release the drug. If the bacteria are sensitive to this drug, they will be killed. If otherwise, they secrete beta-lactamase to inactivate the drug. This enzyme acts on the yellow molecule nitrocefin to turn it red.
If the bandage becomes red, the researchers will pass light through the bandage, which stimulates the production of reactive oxygen species from a metallo-organic compound called PCN-224, built on a porphyrin base, and which has high photodynamic properties, releasing a flood of ROS in response to light. These inhibit or weaken the bacteria, increasing their susceptibility to the drug. Thus, the bandage has been proved to accelerate wound healing in mice after introducing both drug-sensitive and drug-resistant bacteria into the wounds.
The experiment
The researchers incorporated all these elements into a cellulose sheet from which they produced the PBA. They then carried out a proof-of-concept experiment to test whether the PBA could sense drug-sensitive and drug-resistant Escherichia coli (E. coli) in the wound and treat it. Mice with wounds on their back were used. The wounds were infected with drug-sensitive and drug-resistant E. coli, respectively, and the PBA was used to treat the wound for 4 hours.
Escherichia coli bacteria close up. Image Credit: Dreamerb / Shutterstock
The findings
The experiments showed that the PBA over the wound infected with drug-sensitive E. coli turned yellow, proving that this senses the infection very well. The survival of these microbes was reduced markedly in the wound treated with PBA. The wound was almost fully healed on day 3, showing that the ampicillin was enough to heal this infected wound. The irradiated wounds in this category were, however, swollen, showing that the ROS could have caused auxiliary damage.
In the other group, the PBA turned red, showing that drug resistance was sensed well. Moreover, a combination of ROS-based PDT and PBA produced better healing in these wounds. Real-time testing on infected tomatoes showed the usefulness of PBA in picking up drug resistance, and the need to use PDT when drug resistance was sensed.
Conclusion
This highly innovative all-in-one system provides a means of visualizing infection, sensing drug resistance, and selectively applying antimicrobial therapies based on the type of organism (drug-sensitive or drug-resistant). This allows real-time monitoring of drug resistance, minimal off-target side effects, avoids the need for microscopy and saves precious time. The time taken for this sensing was only 2-4 hours, and it could pick up 104 CFU/ml, in the case of drug-resistant E. coli – a highly acceptable limit for clinical use. The high performance, the low cost and the ease of use make it a very appealing application for point-of-care treatment.
Journal reference:
Yuhuan Sun, Chuanqi Zhao, Jingsheng Niu, Jinsong Ren, and Xiaogang Qu. Colorimetric band-aids for point-of-care sensing and treating bacterial infection. ACS Central Science. https://dx.doi.org/10.1021/acscentsci.9b01104.