Age related macular degeneration or AMD leads to loss of vision in around 1.5 million people in the United Kingdom and millions of others around the world. In a new study researchers have discovered a new protein that could explain the causation and thus provide clues to its early diagnosis and effective treatment. The study was published in the latest issue of the journal Nature Communications.
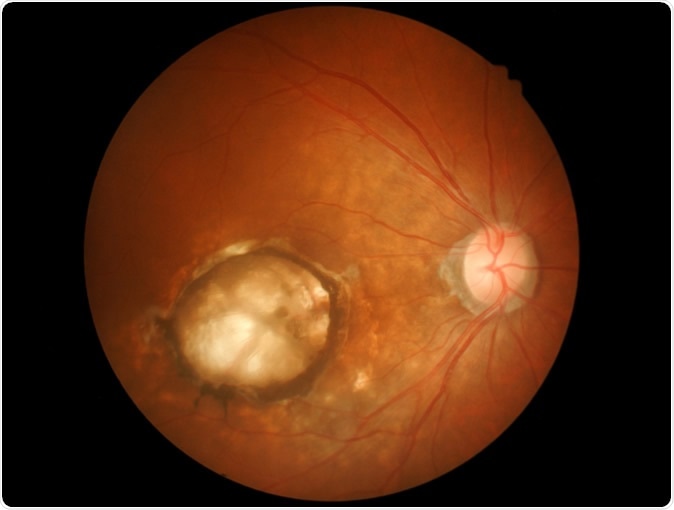
Age-related macular degeneration (AMD). Memorisz / Shutterstock
The researchers from Queen Mary University of London, the University of Manchester, Cardiff University, and Radboud University Medical Center, Nijmegen, collaborated to look at a specific protein called the H-related protein 4 (FHR-4) present in the blood of patients with AMD. They also noted that the levels of this protein were found to be higher among the macular tissues that had been donated by AMD patients for research. Macula is a highly sensitive part of the retina of the eyes that is usually affected by AMD. If the correction holds true, say the researchers, this could open up avenues in detection of AMD by estimation of the level of this protein FHR-4 in blood. This protein formation could also be targeted to treat AMD, they explained.
The team explained that the FHR-4 protein regulates the complement system and is made by genes that are located in the chromosome 1 in a tight cluster. They found that the genes that raise the amount of FHR-4 also were responsible for a higher risk of AMD. It has been known that AMD usually has a genetic origin and certain key complement proteins are involved in its risk and progression. For this study the team looked at the genetic association of the disease with the levels of FHR-4 found in AMD patients. Higher levels of this protein were found in persons who had genetic markers that coded for the H family of proteins. These genes that code for the H proteins usually are found in a single region of the genome, explain the researchers. Certain genetic variants that are closely associated with AMD were also noted in this new genomic study.
The team found that alteration of these genes led to higher levels of FHR-4 that led to cascade of events including activation of the complement system within the eye that leads to start and progression of AMD. For this study they looked at 484 patients with AMD and compared the levels of their FHR-4 with 522 control samples who were age matched with the patients. The patients were recruited from two different sites. The first was from the Cambridge AMD study led by Professor Anthony Moore from Moorfields Eye Hospital and the UCL Institute of Ophthalmology (now at the University of California San Francisco) and Professor John Yates from Cambridge University. The second was from the European Genetic Database (EUGENDA), led by Professor Anneke den Hollander and Professor Carel Hoyng from Radboud University Medical Center.
According to Dr Valentina Cipriani, one of the statistical data analysis experts on the study at Queen Mary University of London, and member of the International AMD Genomics Consortium (IAMDGC), said, “By unveiling FHR-4 as a novel, key molecular player for AMD, our study was able to dissect further the genetic disease predisposition at the factor H region. This is one of the most established genetic associations in the field of complex genetics. We hope our findings will accelerate interest from the wider research community in the involvement of the complement system in AMD, with the ultimate goal of uncovering the role of the whole 'complementome' in the disease.”
Professor Paul Bishop from the University of Manchester and Consultant Ophthalmologist at Manchester Royal Eye Hospital, one of the study leaders said, “The combined protein and genetic findings provide compelling evidence that FHR4 is a critical controller of that part of the immune system which affects the eyes. We have shown that genetically determined higher blood FHR4 levels leads to more FHR4 in the eye which in turn increases the risk of the uncontrolled immune system response that drives the disease.” He added, “So apart from improving understanding of how AMD is caused, this work provides a way of predicting risk of the disease by simply measuring blood levels of FHR4. It also provides a new route to treatment by reducing the blood levels of FHR4 to restore immune system function in the eyes. Because treatments options for AMD are limited, this comprehensive understanding of the biology of AMD is a huge boost for scientists finding answers to a problem which causes untold misery for thousands of people in the UK alone.”
Professor Simon Clark, who co led the study said, “This study really is a step-change in our understanding of how complement activation drives this major blinding disease. Up until now, the role played by FHR proteins in disease has only ever been inferred. But now we show a direct link and, more excitingly, become a tangible step closer to identifying a group of potential therapeutic targets to treat this debilitating disease.”
The study was funded in part by the Medical Research Council and Macular Society and Fight for Sight.
Journal reference:
Cipriani, V., Lorés-Motta, L., He, F. et al. Increased circulating levels of Factor H-Related Protein 4 are strongly associated with age-related macular degeneration. Nat Commun 11, 778 (2020). https://doi.org/10.1038/s41467-020-14499-3