The severity of the disease falls over a wide spectrum, with some having only the mildest of symptoms such as slight fatigue, but others suffering disabling symptoms like joint pain and hair loss, kidney problems and skin rashes.
Types
Lupus occurs in different forms. The systemic form, called systemic lupus erythematosus (SLE) is the most common form and the most serious of all, involving all parts of the body.
Clinical features
Symptoms of lupus include:
- Fever
- Rashes, typically a red butterfly-shaped rash across the nose and cheeks
- Chest pain
- Hair loss
- Sunlight sensitivity
- Nephritis or kidney disease
- Mouth ulcers
- Severe or long-term fatigue
- Anemia
- Blood clots
- Inflammatory eye disease
Complications
The long-term health issues that are more common in women with lupus include:
- Coronary heart disease
- Osteoporosis
- Kidney disease
Staphylococcus and the skin in SLE
Staphylococcus aureus is of minor importance among the organisms which colonize the skin. It is, however, a major pathogen. Its presence in the skin can be detected before the onset of infection. Moreover, interferon production in the skin cells is driven by staph. At the same time, the breakdown of the skin barrier enhances the chances of staph colonization and also promotes lupus disease activity. Staph also causes most cases of bloodstream infection in lupus patients, and having staph on the skin, even without active infection, may increase the number of disease flares and the chances of kidney injury. Thus, staph drives immune system activation.
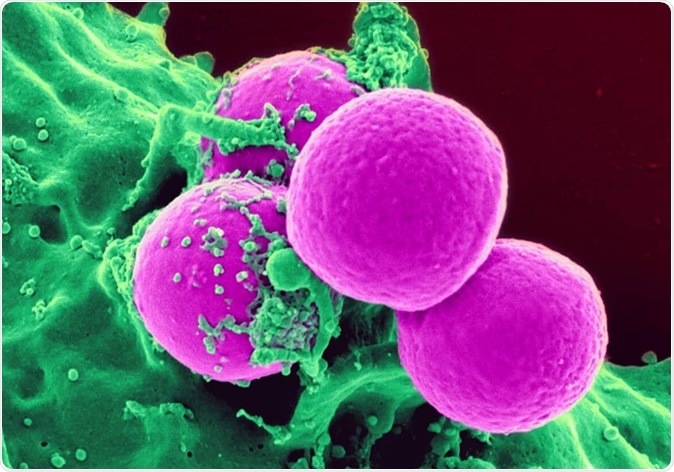
Staphylococcus aureus colony. Image Credit: Ebrahim Lotfi / Shutterstock
The current study
The presence of repeated skin infection in SLE is a common clinical finding, but it’s not clear what drives skin inflammation in this condition. Some of the researchers on the current paper have already carried out studies on skin interferons in patients with lupus, showing its role in causing the characteristic photosensitivity and inflammatory lesions found in lupus.
The present study was motivated by the need to find out if interferons were associated with the presence of staph.
The researchers found that over half of skin rashes in lupus patients were colonized by the common skin-dwelling bacterium Staphylococcus aureus, commonly called staph. This means the bacterium is routinely present on the skin and can be easily transferred to others.
The surprise was the higher level of skin colonization with staph compared to healthy adults, at 40% compared to 30% in the latter. If only active skin lesions were considered, the rate of colonization went up still more, to 50%.
Moreover, lupus patients had high levels of interferon, a protein that is involved in the inflammatory response. As a result, staph is more adherent to the skin in the presence of interferons alpha and gamma, and hence tends to remain on the skin despite washing. However, interferon gamma supressed invasive staph activity.
The study also showed that barrier genes like filaggrin and loricrin are not properly expressed when there is staph infection, leading to a disruption of the normal skin barrier in these patients. Filaggrin loss promotes the formation of natural moisturizing factor, lowers skin pH, and allows the rapid growth of staph colonies. It also enhances photosensitivity and could cause inflammation in response to friendly bacteria or ultraviolet radiation.
Simultaneously, there was an increase in the number of integrins, the skin proteins that promote staph adherence. This indicates increased binding of skin cells in patients with SLE to staph.
These changes commonly found in SLE are also brought about by treating skin cells with interferons. The present study sums up: “Together, these data suggest that chronic exposure to IFNs induces barrier disruption that allows for higher S. aureus colonization in SLE skin.”
Implications
Staph is a common cause of infection in patients with lupus, which led to the researchers bending their focus on this bacterium. Earlier research shows an association between the presence of staph and flare-ups of the disease, as well as with the occurrence of lupus nephritis, or kidney inflammation, in these patients.
Researcher J. Michelle Kahlenberg is now registering patients for a clinical trial to test the beneficial effect of topical antibiotics on the presence of rashes or inflammation in the skin of lupus patients. The effect, if proved, could be a valuable discovery. She says, “This is important because if true, the addition of topical antibiotics may be a simple way to improve treatment response in lupus skin and reduce the ability for those rashes to be colonized by staph.”
Journal reference:
Staphylococcus aureus Colonization Is Increased on Lupus Skin Lesions and Is Promoted by IFN-Mediated Barrier Disruption Sirobhushanam, Sirisha et al. Journal of Investigative Dermatology, https://www.jidonline.org/article/S0022-202X(19)33500-6/fulltext