The brain is among the highest consumers of blood in the human body. In fact, an adult human brain requires about 20% of the energy output of the whole body. However, it is exquisitely dependent on the rest of the body for the energy it needs each moment because it has zero reserve and zero stores. Thus, the cardiovascular system needs to supply the required nutrition every moment.
However, the needs of the brain vary widely depending on the activity level of this organ. Thus, the body needs to gauge the amount of blood it needs at each moment – and not just to the brain overall, but to each part of the brain at any given moment.
This is achieved by an ingenious neurovascular coupling in which blood flow quickly increases to meet the needs of a highly active brain area. In some disease conditions such as high blood pressure, diabetes, and Alzheimer's disease, this process becomes much less sensitive.
Imaging tests like functional magnetic resonance imaging (fMRI) are also highly dependent on the fluctuating blood flow to various brain areas to measure and localize brain activity.
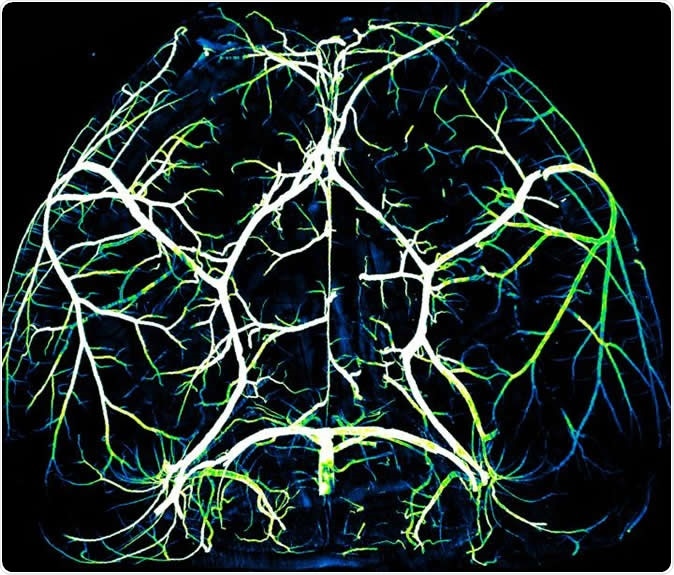
Arteries in the brain. Image Credit: Gu Lab/Harvard Medical School
The importance of neurovascular coupling is thus understandable. Nonetheless, it remained a matter of research as to how the brain communicated with the blood vessels to bring about such a precise and rapid response.
The current study carried out a set of experiments to understand how neurovascular coupling works. They found that the brain's arteries are actively involved in this process of regulating blood flow in response to the levels of a protein called Mfsd2a. This protein has already been discovered to be a vital component of the safety cordon posed by the blood-brain barrier.
Older research by the same investigators showed that the Mfsd2a protein made the blood-brain barrier a strong unit by preventing the formation of tiny lipid bubbles called caveolae, which carry molecular signals. Caveolae originate in the brain capillaries in mice.
However, they also found that arteries, which make up about 5% of brain vessels, did not express this protein, and as a result, they showed large amounts of caveolae. This finding was explored in the current study.
To find out what happens in active areas of the brain concerning blood flow, they used whisker stimulation on live healthy mice who were being imaged for brain activity using 2-photon microscopy.
The findings
The study has done much to uncover changes in the cellular, subcellular, and even molecular components that facilitate neurovascular coupling.
In the first test, the whisker stimulation resulted in increased activity within the brain cells, with the arteries widening and increased blood flow in the sensory cortical area responsible for that sensation. On the other hand, when the test was repeated in mice that were genetically modified to eliminate the caveolae, the neural activity was replicated but not the increase in blood flow nor the arterial widening. The scientists infer that neurovascular coupling was lost in these mice as a result of eliminating caveola production.
Next, the team inhibited the formation of caveolae by specifically suppressing the arterial endothelial cell lining. They did this by inducing the production of Mfsd1a, which is normally absent in these cells, as noted above. The result was the absence of caveolae and, again, weak neurovascular coupling. This proves how important a role is played by the caveolae in this process.
Further experiments showed that the endothelial cells of the arterial lining played a vital and irreplaceable role in this process. When one brain area becomes active, the smooth muscle cells around the arteries relax, causing arterial dilation and more blood flow to that area. On the other hand, there is another way in which neurovascular coupling works independently via caveolae, which transfers the signals to relax from the nerve cells to the smooth muscle cells.
Researcher Brian Chow says, "For over a century, we've known that this phenomenon exists, where neural activity rapidly increases blood flow in a very local and temporally precise manner. But the mechanisms for how the nervous system talks to the vascular system to coordinate this event were largely unknown, and it was astonishing to find that arterial endothelial cells play such an active role in the process."
Another important finding was the fact that the function of caveolae is not a variable of nitric oxide signaling, which is an essential determinant of blood vessel dilation. The well-known medications nitroglycerine, used for congestive heart failure, and sildenafil, for erectile dysfunction, both operate via this pathway.
To test whether this was the case with caveolae, the team suppressed both caveolae formation and the nitric oxide pathway. The result was a complete lack of neurovascular coupling. This means that both these systems are robust but independent processes in blood flow regulation as a result of nerve activity.
However, where caveolae production in arteries regulates sensitive and smaller changes in blood flow, nitric acid may be responsible for more large-scale shifts. Thus the system is not only capable of grossly modulating blood flow but of making the fine adjustments that are characteristic of this regulatory process.
The team is now analyzing the types of signaling molecules within the caveolae to uncover its detailed working. The more they know about it, the better they may be able to construct new experiments to find out its role in health and disease.
As a result of these findings, says researcher Chenghua Gu, scientists can now "dissect this process and determine, for example, whether the neurovascular coupling impairments that we see in diseases like Alzheimer's are the result of pathology or the cause."
Explaining this statement, Gu says, "We've established a very powerful set of genetic tools that allow us to not only identify but manipulate the molecular mechanisms at the heart of neurovascular coupling. For example, even if increased local blood supply is impaired, the brain still has blood flow and oxygen. What is the impact of this on neurons? How does this affect brain function? And does it contribute to conditions like neurovascular dementia? We are now in the position to perform rigorous science that could allow us to answer questions like these."
Journal reference:
Chow, B.W., Nuñez, V., Kaplan, L. et al. Caveolae in CNS arterioles mediate neurovascular coupling. Nature (2020). https://doi.org/10.1038/s41586-020-2026-1