Ulcerative colitis is a seriously debilitating inflammatory disease of the bowel leading to crippling symptoms that can affect the quality of life severely. Researchers from Stanford University School of Medicine have found in a new study that a missing microbe could be linked to this condition. The study was published today in the latest issue of the journal Cell Host & Microbe.
What's the study about?
Researchers explained that a microbe present in the gut could help maintain intestinal health and its absence could raise the risk of ulcerative colitis. Researcher Aida Habtezion, associate professor of gastroenterology and hepatology from Stanford, said, "This study helps us to better understand the disease. We hope it also leads to our being able to treat it with a naturally produced metabolite that's already present in high amounts in a healthy gut." She explained that this microbe raises the levels of a specific metabolite in the gut and thus promotes health. She was assisted in the research by Sidhartha Sinha, assistant professor of gastroenterology and hepatology and Yeneneh Haileselassie, a postdoctoral scholar.
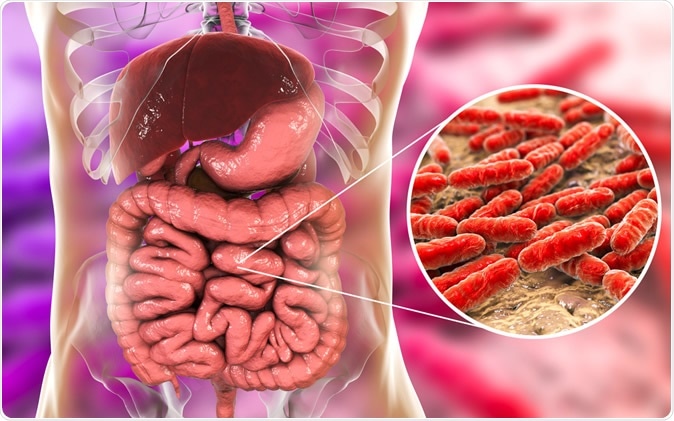
Normal flora of small intestine, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
What was done and what was found?
For this study, the team of researchers compared two groups of patients. One of the groups had ulcerative colitis, and others had a rare non-inflammatory condition of the gut. Both groups had had an identical corrective surgery. Habtezion said, "Patients with a rare genetic condition called familial adenomatous polyposis, or FAP, are at extremely high risk for colon cancer. To prevent this, they undergo the same surgical procedure patients with refractory ulcerative colitis do." These patients acted as controls for the ulcerative colitis patients in this study, she explained.
The team explained that ulcerative colitis leads to inflammation within the gut walls when the body's immune system attacks the cells lining the gut in the rectum and colon. These patients often present with rectal bleeding, diarrhea, and lose weight. At present, treatment involves suppressing immunity using immunosuppressant drugs. These, however, are not always effective, and the disease process can lead to cancers and life-threatening infections. As the next step, these patients require corrective surgery. Surgery may involve total colectomy or removal of the colon and rectum and the creation of a J-shaped pouch from the ends of the small intestine to create a rectum. The pouch again carries a risk of inflammation, and there may be symptoms similar to the initial condition.
Results from this study revealed that those with ulcerative colitis were deficient of a family of bacteria and thus also had low levels of anti-inflammatory substances which are released by the bacterial family within the healthy gut. There were 7 patients with FAP and 17 with ulcerative colitis. The levels of secondary bile acids in those with ulcerative colitis undergoing surgery were significantly lower. Stool samples provided clues about the metabolite content in the gut of these patients.
The team explained that primary bile acids come from the liver and are stored in the gall bladder. They are then released to the digestive tract and help to break down fats. Much of these primary bile acids are reabsorbed in the intestines, and resident bacteria act on them to produce secondary bile acids. Among patients with ulcerative colitis, the levels of these secondary bile acids seem to be lower. Two primary, secondary bile acids noted here in this study were deoxycholic acid and lithocholic acid. They were found to be lower in stool specimens taken from the ulcerative colitis patients with the pouch compared to the FAP patients with a pouch. Since both groups had had the surgery, the cause behind the low levels of the metabolites could not be attributed to the surgery explained by the researchers.
The team also noted that bacterial family Ruminococcaceae was absent or reduced among those with ulcerative colitis. This bacterial family could be assessed using genetic signatures from the samples from the patients, the team wrote. "All healthy people have Ruminococcaceae in their intestines," Habtezion said. "But in the UC pouch patients, members of this family were significantly depleted."
What are the implications?
This study reveals that supplementing the patients of ulcerative colitis with the metabolites or the secondary bile acids produced by this family of bacteria could help correct the symptoms and could soon be developed as a way to manage patients with ulcerative colitis. Habtezion said it could also help patients with other forms of inflammatory bowel disease such as Crohn's disease. They tested this hypothesis on mice models of Crohn's disease, she said.
Way forward
Dr. Sinha, who co-authored this study, is also working on a clinical trial using secondary bile acids in the treatment of ulcerative colitis. Sinha here is the principal investigator, and Habtezion is the co-principal investigator. This is a Phase 2 trial and would include 18 patients with ulcerative colitis of an average age of 70 years. They would all be given oral supplements containing ursodeoxycholic acid, which is a naturally found secondary bile acid and is approved by the Food and Drug Administration (FDA) for treatment of gall stones and primary biliary sclerosis.
Journal reference:
Dysbiosis-Induced Secondary Bile Acid Deficiency Promotes Intestinal Inflammation Sinha, Sidhartha R. et al. Cell Host & Microbe, https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(20)30062-7