A minimal – and therefore innocuous – dose of an antibiotic coupled with highly sensitive measurement technology could save time and money in the development of new active ingredients. The shortcut lies in being able to do pharmacokinetic testing earlier, which consists in establishing proof that the potentially antibacterial agent can actually become effective at its desired site of action.
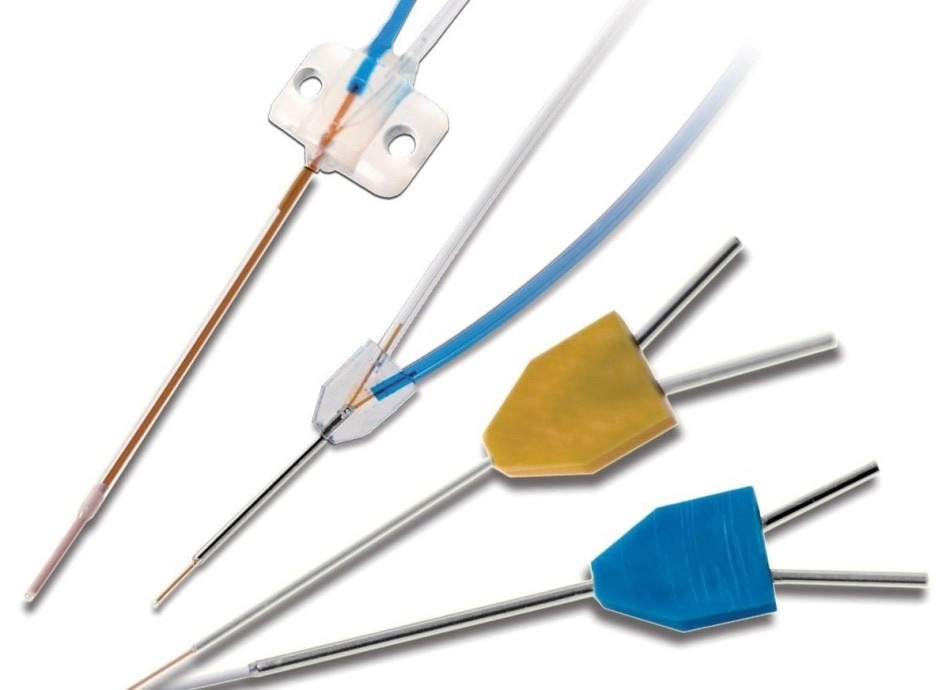
Microdialysis, which involves the insertion of a small probe into the tissue, provides precise measurements of drug effectiveness. This makes the development of vital drugs faster and more efficient. Image Credit: Facaccia, CC BY-SA 3.0.
The statement sounds paradoxical, as the discovery and development of antibiotics was a milestone in medical history and has saved the lives of many people. Nevertheless, many pharmaceutical companies are withdrawing from the field because the development of the active ingredients is not a lucrative undertaking. Antibiotics are effective against bacterial infections and, depending on the active ingredient, kill specific germs quickly. Like all living organisms, bacteria change and can become resistant. In addition, well-established antibiotics are also used carelessly or inappropriately, which means they become increasingly ineffective.
“The development of antibiotics to the point of getting them approved is just as costly as that of cancer drugs. But they are only administered for a short time. Furthermore, new antibiotics are used restrictively against multi-resistant germs, which also brings down revenues,” says the head of the University Clinic for Clinical Pharmacology at the Medical University of Vienna, describing the situation that motivated his project. The good news: in a study, his research group has successfully tested a method for the accelerated development of antibiotics.
Currently, Zeitlinger is also tapping into this knowledge in the search for suitable drugs to combat the coronavirus. In cooperation with different companies and researchers, the physician is working on numerous projects for the accelerated development of already available und promising substances for the fight against Sars-CoV-2.
Pharmacokinetics shortcut
The most common bacterial infections are pneumonia, soft-tissue and urinary tract infections and inflammations in the abdominal cavity following surgery. Funded by the Austrian Science Fund FWF, the study was devoted to finding a shortcut in the development process for two of these four sites where antibiotics are used. “Foci and bacterial biofilms are most frequently located in the lungs or between body cells. Antibiotics therefore need to achieve a certain concentration level in a specific tissue in the human body in order to be able to kill a germ,” is Markus Zeitlinger’s simple explanation of the technical term “pharmacokinetics”. And “pharmacodynamics”, expressed in lay terms, describes whether the germ dies on contact with the antibiotic. In the case of a potential antibiotic, these two factors together enable predictions of its effectiveness, which can speed up the development process and thereby make it more attractive.
Pharmacodynamics is tested in vitro using conventional methods. Before testing pharmacokinetics (i.e. whether the active ingredient will reach the desired site of action), animal testing is carried out to ensure that the substance is harmless to the human body. The project team were able to show that the pharmacokinetics for the lung and soft tissue can be demonstrated with harmless microdosing and highly sensitive detection methods. In the future, this would make it possible to decide more quickly whether an active ingredient should undergo further testing or be discarded.
Same kinetics at minimum dosage
In the two-year clinical research project (2017-2019), pharmacokinetics in the target tissues were tested on the basis of an already approved drug. This is the question the research team set out to answer: would it have been possible to develop this antibiotic using the new approach? Upon giving their informed consent, 18 healthy volunteers were administered the antibiotic ciprofloxacin intravenously. The volunteers received one normal dose and one definitely harmless microdose marked with radioactive C14. Despite the low concentration, the marker allows the active ingredient to be detected in the lungs and soft tissue by means of accelerated mass spectrometry (AMS).
In order to detect the pharmacokinetics in the tissue, the researchers performed lung lavage (Broncho Alveolar Lavage/BAL) on the sedated test persons and determined the concentration level of the active ingredient in the fluid flushed from the lungs. A microprobe in the thigh (microdialysis) was used to measure how much freely available antibiotic was contained in the fluid between the tissue cells to kill off the germs. Only three institutions in the world have an AMS measuring device that can detect two radioactive atoms in a prepared shovelful of soil. The University Hospital in Vienna cooperated with the TNO Institute in Zeist (The Netherlands) for the tests.
Early prediction of effectiveness
The clinical trial has already been completed and all test persons are doing well.
By means of microdialysis, we were able to show that pharmacokinetics can be described well even by a harmless microdose which was proportional to that of the conventional dose – i.e. independent of the amount of active ingredient.”
Markus Zeitlinger
It was also possible to establish the site of action for the lung lavage fluid. The exact correlation is currently being measured a second time. If the prediction of the effectiveness of the drug can be achieved accurately with a fraction of the usual dose, pharmacodynamics can be simulated and refined in order to determine the effective dose. “In this way, we hope to speed up research on essential drugs and thus make it more attractive and efficient. The combination of microdosing and tissue pharmacokinetics can save up to two years and two million euros in the development of potential antibiotics,” says the clinical pharmacologist. In a future study, his team will examine whether the microdosing concept can also be used to test an ointment.