Researchers working on a National Institutes of Health (NIH) funded study found that polycystic ovary syndrome (PCOS) has distinct subtypes that are associated with genetic variations. Their study titled, "Distinct subtypes of polycystic ovary syndrome with novel genetic associations: An unsupervised, phenotypic clustering analysis," is published in the journal PLOS Medicine.
Polycystic ovary syndrome
PCOS affects a large number of women, and authors of the study explain it as a "common, complex genetic disorder." They write that as many as 15 percent of women of reproductive age group suffer from this condition, and several diagnostic criteria can help in confirming the condition in a patient.
In women with PCOS, some of the common symptoms include irregular or missing periods, lack of or infrequent ovulation, raised levels of male sex hormones – androgens in blood and associated features such as hirsutism or excessive facial hair. On ultrasound investigation, small cysts are detected on the surface of the ovaries. These women are at risk of being overweight and obese and may develop heart disease and type 2 diabetes and metabolic syndrome with time.
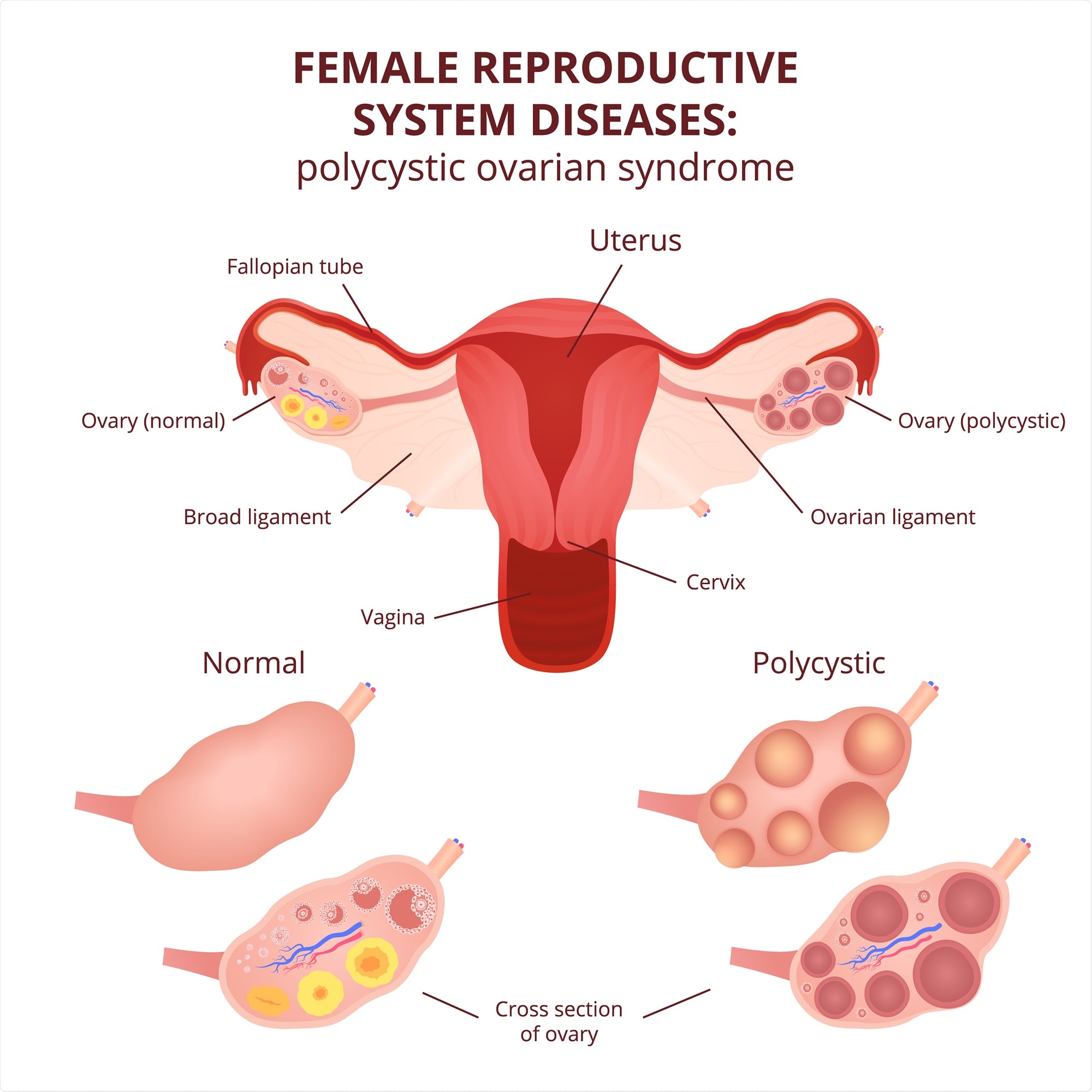
Image Credit: Marochkina Anastasiia / Shutterstock
What was this study about?
There are several diagnostic criteria for the detection of PCOS. These are mainly based on expert opinions and consensus. Several controversies exist in these diagnostic criteria for PCOS, the team wrote.
There is a variation of physical features and physical symptoms among patients with PCOS. These are called phenotypic variations. In a recent study across populations with European ancestry, it was noted that the genetic makeup of women suffering from PCOS was distinctly similar despite being labeled using different diagnostic criteria. They write that this suggests that these diagnostic criteria "do not identify biologically distinct disease subtypes."
The objective of this study was thus to "test the hypothesis that there are biologically relevant subtypes of PCOS." Researcher Andrea Dunaif, MD, Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes and Bone Disease at the Mount Sinai Health System, explained, "We're starting to make headway on what causes PCOS. It's very frustrating for patients because it's poorly understood, and patients often see several physicians before PCOS is diagnosed." Dunaif added, "Through genetics, we're beginning to understand the condition and may have specific targeted therapies in the not-too-distant future."
What was done?
Study participants were a genotypical cohort. The biochemical data and the genotype data from these women was obtained from the "PCOS genome-wide association study (GWAS)." They made connections with the genotypes and the phenotypic or physical subtypes of the condition. A total of 893 women were included in the study. Their age range was between 25 and 32 years, and body mass index was between 28.2 and 41.5. These genotypic clusters were replicated in another cohort, which were not genotyped. Here there were 263 PCOS cases with an age range of 24 to 33 years and BMI ranging between 28.4 and 42.3.
What was found in the study?
PCOS subtypes
On clustering analysis, the team found two distinct subtypes of PCOS. These were –
- The reproductive group, roughly 23 percent of participants, was typically characterized by raised levels of luteinizing hormone (LH) and sex hormone-binding globulin (SHBG). These participants also had low BMI and low insulin levels.
- The Metabolic group, roughly 37%, had a higher BMI, raised levels of blood sugar and insulin but lower levels of LH and SHBG.
Genetic findings
On genotyping the initial cohort and dividing them into the two types of PCOS, several genetic characteristics were detected. The findings were:
- Alleles were found in 4 loci seen in the reproductive subtype of PCOS. These were, “PRDM2/KAZN, P = 2.2 × 10−10; IQCA1, P = 2.8 × 10−9; BMPR1B/UNC5C, P = 9.7 × 10−9; CDH10, P = 1.2 × 10−8”
- One loci was significantly seen in the metabolic subtype – "KCNH7/FIGN, P = 1.0 × 10−8".
Family clusters
A separate predictive model was developed to see if the cases tended to cluster in families. They found that 73 women with PCOS within an age range of 25 and 33 and BMI range of 27.8 and 42.3 kg/m2, usually "tended to cluster in families and that carriers of previously reported rare variants in DENND1A". The team wrote that this gene variant is known to regulate the synthesis of androgens or male hormones in the body.
Limitations of the study
The authors said that this initial study was conducted only among women with European ancestry who were diagnosed based on the National Institutes of Health (NIH) criteria. More extensive studies with a wide-ranging population would be more conclusive.
Conclusions and future implications
The researchers wrote that they "found reproducible reproductive and metabolic subtypes of PCOS," and these subtypes were "associated with novel, to our knowledge, susceptibility loci." They wrote that these subtypes had distinct genetic architecture.
Dr. Dunaif said, "In contrast to classifying disorders based on expert opinion, this is a very powerful objective approach to categorizing syndromes like PCOS into distinct subtypes with different causes, treatment, and clinical outcomes."
The team wrote, "Women with PCOS may be poorly served by being grouped under a single diagnosis because PCOS subtypes may differ in responses to therapy and in long-term outcomes."
Journal reference:
- Distinct subtypes of polycystic ovary syndrome with novel genetic associations: An unsupervised, phenotypic clustering analysis, Dapas M, Lin FTJ, Nadkarni GN, Sisk R, Legro RS, et al. (2020) Distinct subtypes of polycystic ovary syndrome with novel genetic associations: An unsupervised, phenotypic clustering analysis. PLOS Medicine 17(6): e1003132. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003132