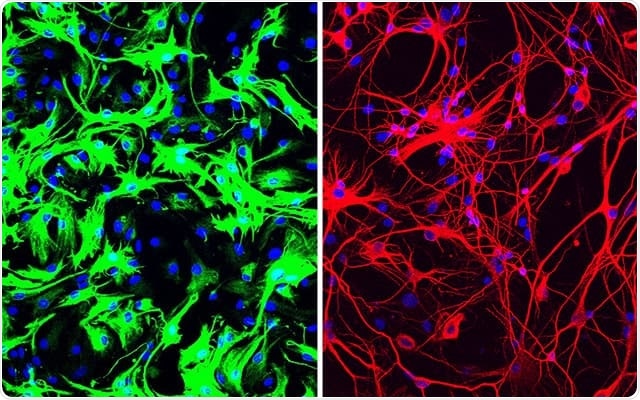
Left: mouse astrocytes (green) before reprogramming; Right: neurons (red) induced from mouse astrocytes after reprogramming with PTB antisense oligonucleotide treatment.
Parkinson's disease is a neurodegenerative disorder typically characterized by loss of cells in the substantia nigra of the brain. This region produces the essential neurotransmitter dopamine that can connect the substantia nigra with the corpus striatum to regulate muscle activity. This dopamine deficiency can lead to excessive "firing" of the nerve cells, and thus the individual loses direct control over movements. With time, several regions of the brain experience degeneration of the neurons, and this leads to a more profound movement disorder. Both genetic and environmental factors contribute to Parkinson's disease. Following symptoms are most commonly seen among patients with Parkinson's disease:
- The slowness of movement (also known as bradykinesia)
- Tremor or shaking movements seen at rest
- Muscle rigidity and increased tone of the muscles.
The astrocytes rewritten into dopaminergic nerve cells
In the mouse model, the team of researchers successfully created new neurons or nerve cells. This was done using a simple method of rewriting the genes of the animal, the team explained.
Led by researcher Xiang-Dong Fu, professor of cellular and molecular medicine at UCSD, this study could help cure Parkinson's disease one day. The team explained that brain cells called astrocytes were converted into functioning dopaminergic cells, which were lost due to Parkinson's disease. This replacement of the damaged cells helped in regaining the lost abilities. The rewritten cells were implanted into the brain, and they functioned normally reversing the symptoms.
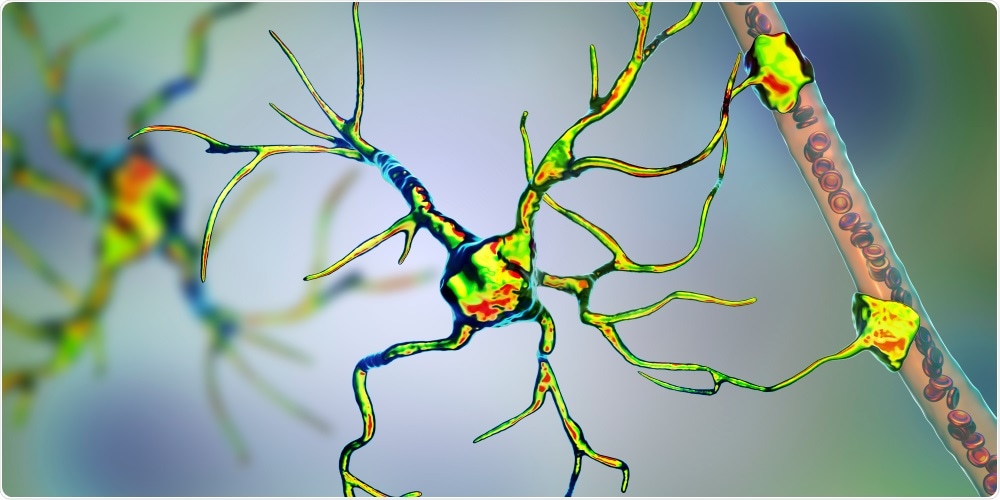
Astrocyte and blood vessel, 3D illustration. Astrocytes, brain glial cells, also known as astroglia, connect neuronal cells to blood vessels. Image Credit: Kateryna Kon / Shutterstock
The scientists experimented on isolated human cells as well as lab mice. The newly made neurons were implanted on the mice with the motor symptoms of Parkinson's disease. They were directly implanted into the areas depleted of the dopaminergic neurons.
How did they do it?
The researchers explained that astrocytes produce a unique protein that prevents them from becoming nerve cells or neurons. The team of researchers simply stopped the production of this protein by astrocytes, to coax them into becoming dopaminergic neurons. They noted that these newly formed neurons then repopulated all the depleted brain circuits that had occurred due to the degenerative disease. This helped raise the dopamine levels, and finally, the motor functions were reversed in the mice with Parkinson's disease. The team used "PTB antisense oligonucleotide treatment," to create these new neurons from the astrocytes.
What was found?
After injecting the newly made neurons, the dopaminergic neurons rose by 30 percent among the treated mice. Their dopamine levels also rose to normal, the team explained. After a single treatment, the mice had regular motor movements in around three months. For the rest of their lives, they remained free of all symptoms of Parkinsonism. The control group of mice showed no such improvement.
William Mobley, a UCSD neurosciences professor, said, "I was stunned at what I saw. This whole new strategy for treating neurodegeneration gives hope that it may be possible to help even those with advanced disease."
Future potential
Researcher Xiang-Dong Fu in a statement, said, "It's my dream to see this through to clinical trials, to test this approach as a treatment for Parkinson's disease, but also many other diseases where neurons are lost, such as Alzheimer's and Huntington's diseases and stroke."
Dr. Fu added, "'Researchers around the world have tried many ways to generate neurons in the lab, using stem cells and other means, so we can study them better, as well as use them to replace lost neurons in neurodegenerative diseases...The fact that we could produce so many neurons in such a relatively easy way came as a big surprise."
The researchers, however, warn that it may be some time before more research comes in, and the approach could be applied to human patients with Parkinson's disease.
Ernest Arenas, a neuroscientist at Sweden's Karolinska Institute, added that the simplicity of the technique was what was unique about this study. He said, "Just by removing a brake on these cells by suppressing the PTB gene, they were ready to go and make neurons."
According to Professor Tara Spires-Jones of the UK Dementia Research Institute at the University of Edinburgh and deputy director of the Centre for Discovery Brain Sciences, University of Edinburgh, this study is an important one. She said, however, "It is important to note that it was conducted in mice with group sizes from three to eight, and there is a long way to go to translate this into a treatment for people."
Robert Howard, professor of geriatric psychiatry from University College London called this an "extraordinary scientific discovery" and said, "This opens up a completely novel avenue for the development of treatments to 'rebuild' damaged brains in Alzheimer's and Parkinson's diseases."