Drugs that were developed to treat Alzheimer’s Disease could be re-purposed to prevent - or even reverse - the damage done to the blood vessels in people who are obese or suffer from type 2 diabetes, according to new research.
People suffering from a range of conditions called metabolic syndrome – which includes type 2 diabetes, high blood pressure, high cholesterol and obesity – have a stiffening of their blood vessels that puts them at increased risk of a heart attack or stroke.
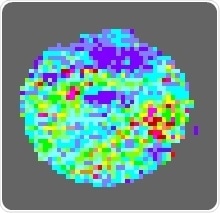
The image shows the blood flow in the surface blood vessels of a mouse that was given M-3.
In a breakthrough, scientists at the University of Leeds and University of Dundee have discovered a key mechanism that triggers changes in the blood vessels, which can eventually lead to cardiovascular disease.
It starts when people begin to overproduce an enzyme called BACE1 which in turn creates a protein called beta amyloid.
Raised levels of beta amyloid are associated with damage to the surface lining of blood vessels, the endothelium. This disrupts the normal functioning of the blood vessels leading to high blood pressure and atherosclerosis, the build-up of plaque along the walls of the blood vessels.
We know that people living with diabetes are at higher risk of heart attacks or stroke, but we don’t yet know exactly why. The new research helps to shed light onto the connection. If the enzyme BACE1 is responsible for this increased risk, it represents a promising target for new treatments, which could help people with diabetes live longer, healthier lives.”
Eddie Johnston, Diabetes UK
Published today (Monday, June 29th) in The Journal of Clinical Investigation, the findings are the culmination of eight years of research, which started at Dundee and then expanded to Leeds and involved both human and animal studies.
The animal investigations looked at the effect of an experimental compound called M-3, which stops the actions of BACE1. In studies on mice that were obese or had diabetes, it was shown to not only to halt disease in the blood vessels - but to reverse it.
The attached images were taken from laser scans of the skin of mice with diabetes. They show blood flow through the small blood vessels in the skin. The blue colors signify low blood flow. Red, yellow and green colors, represent higher blood flow.
Image one was from an animal that had not been given M-3, and indicates a problem with blood flow. Image two, was from a mouse that had received M-3, and it shows improved blood flow.
Dr Paul Meakin, University Academic Fellow in the Leeds Institute of Cardiovascular and Metabolic Medicine, was the paper’s lead author. He said: “The therapeutic effects of the experimental compound were marked, with the progression of disease in badly damaged blood vessels being reversed.”
He added: “Sometimes in science you look at the data you produce and there is the hint of something there – but the effects that we observed were dramatic.
“And the most exciting thing is that there are drugs that can target the BACE1 enzyme.
“It opens up the possibility that scientists can develop a medicine that inhibits the actions of BACE1 – with the evidence suggesting that it may not only halt the progress of disease in the blood vessels but could reverse it.”
BACE1 and the links with Alzheimer’s disease
BACE1 has previously caught the attention of the pharmaceutical industry because of its role in the development of another major illness, Alzheimer’s Disease. BACE1 is directly linked with the development of beta amyloid plaques found in the brains of people who died with the condition.
Drug companies have started developing BACE1 inhibitors – so far, they have been ineffective in tackling Alzheimer’s.
Mike Ashford, Professor of Neuroscience at the University of Dundee, supervised the research that has just been published. He said: "Our work demonstrates that an early abnormal biological process, which is strongly linked to Alzheimer’s disease, may be responsible for vascular disease and hypertension in people with obesity and diabetes."
"These findings suggest the exciting possibility whereby existing drugs that have unfortunately shown no benefit in clinical trials for Alzheimer’s Disease, may instead be used to treat vascular disease in this group of people."
Blood vessel damage caused by diabetes accelerates and worsens heart and circulatory diseases. These findings identify a new damaging pathway already targeted by a drug in development for the treatment of Alzheimer’s Disease. This drug now needs to be tested in people with diabetes in the hope it has the ability to reduce the progress of heart and circulatory disease in the millions of people living with diabetes in the UK.”
Professor Jeremy Pearson, Associate Medical Director at the British Heart Foundation
The research was funded by grants from the British Heart Foundation, Diabetes UK, the Medical Research Council, the Diabetes Research and Wellness Foundation, and the Innovative Medicines Initiative (SUMMIT).