Dementia rates have been increasing at an alarming rate around the world. In fact, some researchers have reported a higher incidence of dementia in women as compared to men, with certain reproductive factors associated with an increased risk of dementia. However, hormone use in women and their associations with dementia risk remains unclear.

Study: Reproductive factors and the risk of incident dementia: A cohort study of U.K. Biobank participants. Image Credit: pikselstock / Shutterstock.com
Background
Fifty million people live with dementia globally and this number could triple by 2050. Mitigation and modification of risk factors could reduce the burden associated with dementia at a population level, given that there are no effective course-modifying treatments for dementia to date.
The rates of dementia have been estimated to be higher in women; however, the extent to which this associated is due to women’s longer life span remains to be determined. Female-specific reproductive factors could potentially explain these sex disparities.
During the course of a woman’s reproductive life, several endogenous estrogen changes occur. Exogenous hormone use, such as oral contraceptives, and hormone replacement therapy (HRT) can influence estrogen levels.
To date, there is a lack of research that studies the long-term effect of reproductive factors on dementia risk. The putative mechanisms are unclear and the conclusions remain far from being certain.
About the study
In the new cohort study, researchers studied women in the U.K. Biobank and examined the reproductive factors and exogenous hormone use in relation to the risk of incident all-cause dementia. The association between these factors and the risk of dementia was studied and correlated with a range of factors such as age, socioeconomic status (SES), smoking status, and BMI.
Additionally, men were also included for a between-sex comparison. The association between the number of children these men fathered and the risk of all-cause dementia was assessed and compared to the results obtained from their female counterparts.
Study findings
Scientists observed several associations between reproductive factors and exogenous use of hormones with the risk of dementia. Younger age at first live birth and hysterectomy was associated with a greater risk of dementia.
A U-shaped relationship was found between the risk of dementia and several factors including age at menarche, hysterectomy, and oophorectomy. Lower risk of dementia was associated with a longer reproductive span, late natural menopause, being pregnant at some points, and a history of abortion.
In the case of exogenous hormone exposures, the use of oral contraceptive pills was associated with lower dementia risk. Women who had a lower SES were found to be at an elevated risk of dementia. Among both sexes, a U-shaped association was found between the number of children and the risk of dementia.
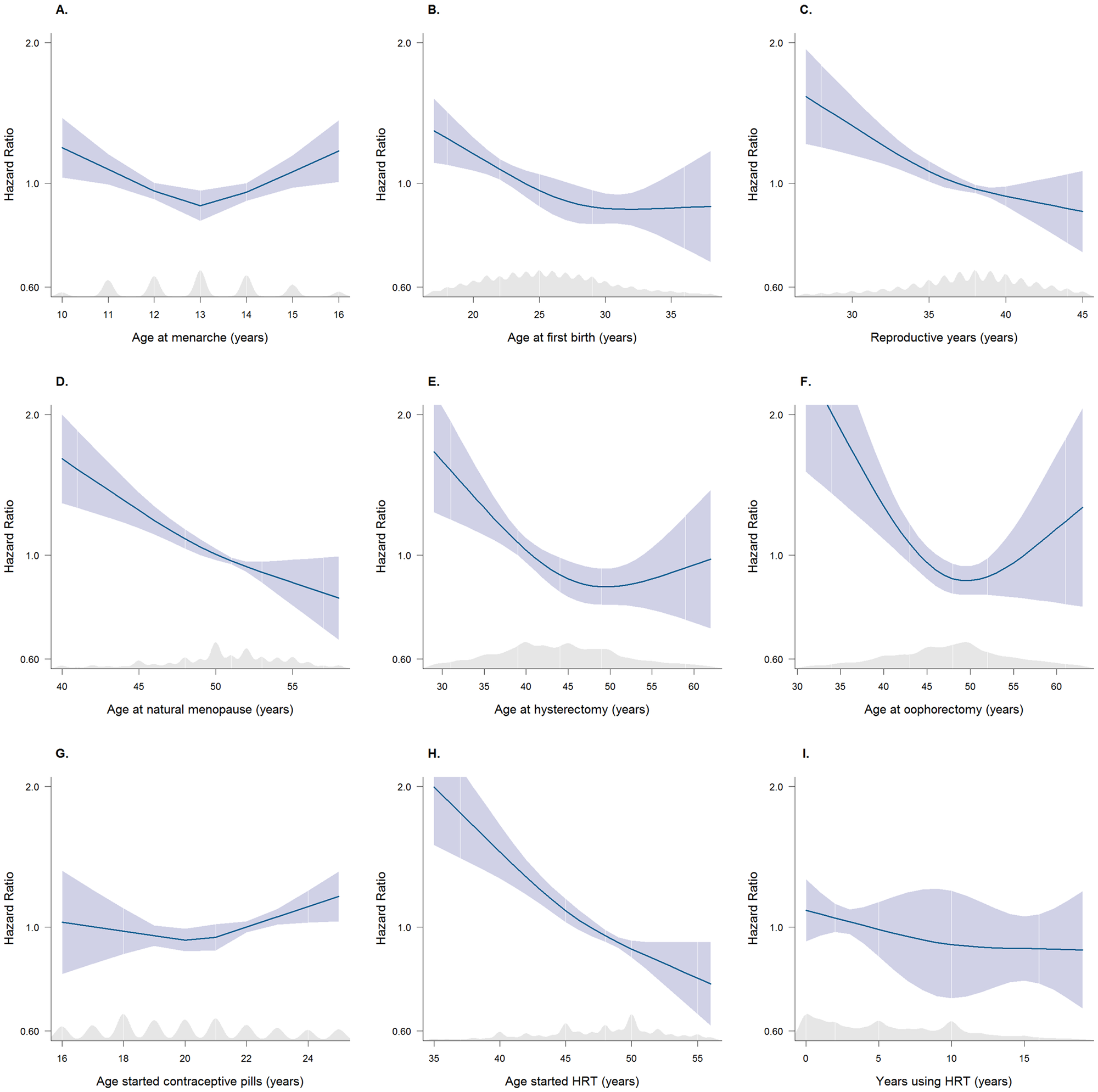 Multiple adjusted restricted cubic splines (with kernel density plots) showing HRs for the risk of dementia associated with reproductive factors. The blue line represents the hazard function, and the blue shaded area represents the 95% CIs. The shaded grey region represents the kernel density plot for the distribution of data. After excluding the values from the top and bottom 2.5% of the distribution, with the median value being the reference. Splines adjusted for age, Townsend deprivation index, ethnicity, smoking status, systolic blood pressure, BMI, diabetes, total cholesterol, antihypertensive drugs, and lipid-lowering drugs. (A) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at menarche. (B) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at first birth. (C) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with reproductive years. (D) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at natural menopause. (E) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at hysterectomy. (F) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at oophorectomy. (G) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age-started contraceptive pills. (H) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age started HRT. (I) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with years using HRT. BMI, body mass index; CI, confidence interval; HR, hazard ratio; HRT, hormone replacement therapy.
Multiple adjusted restricted cubic splines (with kernel density plots) showing HRs for the risk of dementia associated with reproductive factors. The blue line represents the hazard function, and the blue shaded area represents the 95% CIs. The shaded grey region represents the kernel density plot for the distribution of data. After excluding the values from the top and bottom 2.5% of the distribution, with the median value being the reference. Splines adjusted for age, Townsend deprivation index, ethnicity, smoking status, systolic blood pressure, BMI, diabetes, total cholesterol, antihypertensive drugs, and lipid-lowering drugs. (A) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at menarche. (B) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at first birth. (C) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with reproductive years. (D) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at natural menopause. (E) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at hysterectomy. (F) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age at oophorectomy. (G) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age-started contraceptive pills. (H) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with age started HRT. (I) Restricted cubic spline plot with multiple adjusted HRs (95% CI) for all-cause dementia associated with years using HRT. BMI, body mass index; CI, confidence interval; HR, hazard ratio; HRT, hormone replacement therapy.
Strengths and limitations
Large sample size with linkage to national health records and death registers is one of the key strengths of this study. The data also included a comprehensive list of reproductive factors and exogenous hormone use, which was an additional strength.
Retrospective and self-reported measures of reproductive factors, which may be subject to bias, are one key limitation of the study. The U.K. Biobank population primarily consists of relatively healthy and affluent people of white ethnic background, which is therefore limited in terms of its representativeness.
Furthermore, dementia subtypes were not differentiated due to the small number of events in the U.K. Biobank. A final limitation was that, despite the best attempts by researchers, some unmeasured factors could lead to residual confounding.
Conclusions
The current study highlights that various reproductive and hormonal factors in women may be associated with an increased risk of dementia. For example, SES could be an important determinant of dementia risk and other aspects of women’s health.
Given the similar observed association between the number of children and dementia in both sexes, the physical experience of childbearing is unlikely to account for the risk variation in women.
Taken together, the current study supports a life course approach for dementia prevention. Herein, the scientists provide new insights into potential strategies that can be used to reduce the risks of dementia associated with certain reproductive factors that are unique to women. In the future, the findings on exogenous hormone use should be validated by rigorous clinical trials, while also identifying high-risk women for future trials.
Journal reference:
- Gong, J., Harris, K., Peters, S. A. E., & Woodward, M. (2022) Reproductive factors and the risk of incident dementia: A cohort study of U.K. Biobank participants. PLoS Medicine 19(4). doi:10.1371/journal.pmed.1003955.