Please can you introduce yourself and tell us about your background in biomedical engineering, as well as what interested you in conducting this research?
My name is Aitor Aguirre, and I am an Assistant Professor of Biomedical Engineering at Michigan State University. My lab applies engineering approaches to study how the human heart forms and responds to injury, with the goal of applying this knowledge to new regenerative medicine-based therapeutics.
We conduct studies on heart regeneration because although humans do not regenerate the heart, other animals close to us do, suggesting we might have a dormant capacity in this respect. This is supported by the fact that upon injury, our heart does mobilize stem cells to repair itself; however, their work is insufficient as there are too few of them. We are trying to find ways to boost these stem cells.
We stumbled upon oxytocin accidentally. We were looking for important neurohormones that might exert control over heart regeneration and testing dozens of them when we found that oxytocin had very powerful effects. That is how this research started.
 Image Credit: designium/Shutterstock
Image Credit: designium/Shutterstock
Can you tell us more about oxytocin and what its main functions are within the body?
Oxytocin is a neuropeptide involved in social bonding and pleasure. It is stored in the hypothalamus, in the brain. We release oxytocin when we see someone we love or do something we enjoy. However, oxytocin has other biological roles, some of them still poorly understood.
Your research utilized zebrafish and human cell cultures to demonstrate that oxytocin has another surprising function. Can you tell us about how you conducted your study, as well as the unexpected findings you established?
We performed a screening for neurohormones involved in body homeostasis in human epicardial cells. Epicardial cells are a population of epithelial cells living on the surface of the heart. Still, they are also known as a reservoir of stem cells that can repair the heart (although found too rarely to help significantly).
Since regeneration is a very energetically demanding process, we reasoned there should be some brain-related central control on this process.
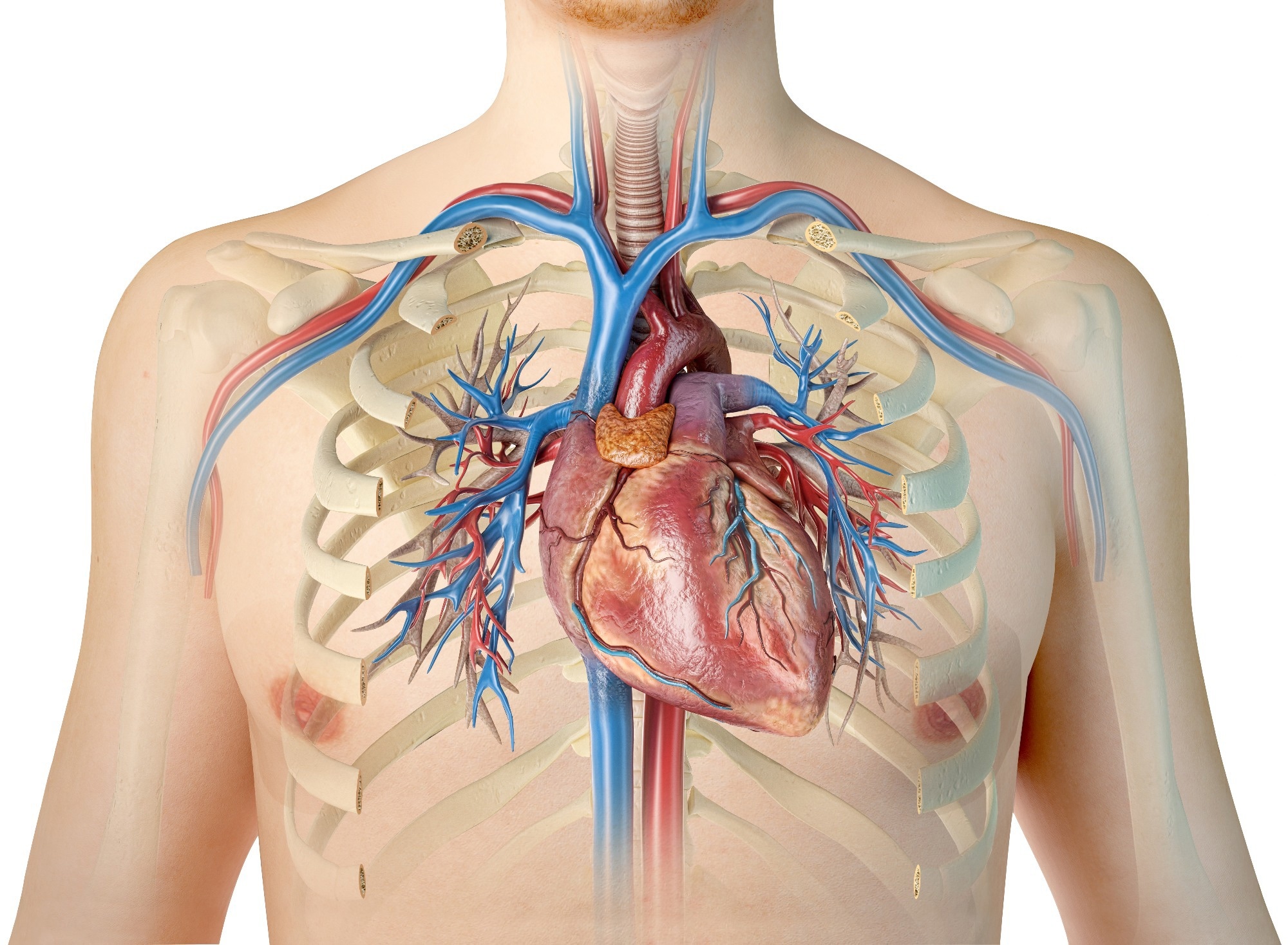 Image Credit: Matis75/Shutterstock
Image Credit: Matis75/Shutterstock
We found that oxytocin boosted the ability of epicardial cells to turn into epicardial stem cells and proliferate. We then moved to zebrafish, a well-established regeneration model, to see if the effects of oxytocin were conserved. We found that removing oxytocin severely limited the regeneration ability of the fish and the formation of epicardial stem cells, confirming our hypothesis.
Zebrafish may be able to teach us how to regenerate hearts more efficiently. What are some of the advantages of using zebrafish in research like yours?
The zebrafish is one of the most powerful regenerating vertebrates, it can make a new brain, heart, bones, muscles, et cetera without any loss of function. Since it is relatively close to us (it is a vertebrate, after all), many of the cellular and molecular events leading to this extraordinary healing capacity are present in us too. The question is, why can they do it and we cannot?
 Image Credit: Ian Grainger/Shutterstock
Image Credit: Ian Grainger/Shutterstock
How do you believe your findings could open the door to potential new therapies for heart regeneration in humans?
These findings indicate that oxytocin, or a drug that mimics its effects, might have positive effects in patients that underwent a myocardial infarction event by regenerating parts of the lost muscle. Even if this treatment is only partially successful (let’s say only 15% of the damaged muscle comes back), it is still a huge step forward from a clinical perspective that would significantly improve patients' lives. It will also pave the way for more sophisticated approaches, maybe combined with other drugs or pro-regenerative factors, to improve regeneration even more.
What is next for you and your research to move forward?
For this project, the next step will be pre-clinical trials in relevant animal models to determine safety and efficacy. If the results are positive, I would envision clinical trials in the near future to develop a medication based on this approach.
Where can readers find more information?
Link to the study: https://www.frontiersin.org/articles/10.3389/fcell.2022.985298/full
Link to Dr. Aguirre's lab: https://www.aguirrelab.org/
About Aitor Aguirre
Dr. Aguirre obtained his M.Sc. in Biochemistry and Molecular Biology at the University of the Basque Country and his Ph.D. in Material Science and Tissue Engineering at the Institute for Bioengineering of Catalonia (IBEC) and the Technical University of Catalonia (UPC). For his postdoctoral training Dr. Aguirre worked at The Salk Institute, where he explored in vivo reprogramming applied to cardiac regeneration. Dr. Aguirre became Assistant Professor of Medicine at the University of California, San Diego in 2017 and joined the Institute of Quantitative Health Science and Engineering and the Department of Biomedical Engineering at Michigan State University one year later. Dr. Aguirre has extensive experience in cardiac development, cardiovascular disease, regenerative medicine and tissue engineering.
regeneration. Dr. Aguirre became Assistant Professor of Medicine at the University of California, San Diego in 2017 and joined the Institute of Quantitative Health Science and Engineering and the Department of Biomedical Engineering at Michigan State University one year later. Dr. Aguirre has extensive experience in cardiac development, cardiovascular disease, regenerative medicine and tissue engineering.