At MEDICA 2022, NewsMedical spoke with Heike and Thorsten Walles, co-founders of MD2B LifeScience, which provides realistic thorax models for surgical and implant training. These 3D-printed models could revolutionize how training is approached, with replaceable ribs that replicate the behavior of actual human bones.
Please could you introduce yourselves and your professional backgrounds?
Heike Walles (HW): My name is Heike Walles. I'm a biologist and I've worked for 25 years in the field of tissue engineering. I have a lot of experience in how you can combine materials with cells to create tissue-specific models.
Thorsten Walles (TW): My name is Thorsten Walles. I am a surgeon specializing in thoracic surgery, and I'm the professor for thoracic surgery at the University of Magdeburg, where I train young doctors. I'm also involved in training programs with our National Society for Thoracic Surgery.
MD2B LifeScience is a spin-out from Magdeburg University that creates 3D-printed thorax models for medical training and surgical planning. What inspired you to pursue a thoracic modeling solution?
TW: It started with one robotic surgery. When we use robotics, the surgical procedures are very standardized, but I wanted to do a non-standardized approach for a rare tumor and had the problem of how I could rearrange the robotic setting for my patient. At that point, I wished that there would be some kind of training device to just play around a little bit with how to plan the surgery, but unfortunately, there wasn't. So I did the surgery without training, and everything went fine, but that launched the idea where everything started.

Image Credit: MD2B LifeScience
I asked the Engineering Department at our University whether it would be possible to generate some 3D thorax models, and the engineers told me that they could do it.
What was the development process like for your thorax models, and how have they evolved since your initial ideas?
TW: It turned out that technically there were some challenges that the engineers had to solve, which they did. Then the idea continued so we decided to create a model for training young doctors and even professionals like me for complicated surgeries.
We introduced our idea in September 2021 to a national medical congress, and then other doctors had additional ideas. Then, some industrial representatives remarked, 'well you have the chest and you have the bones of the chest; this is useful for our implants.' They realized that they could use the models for training on applying implants or modifying implants. And so the idea kept growing.
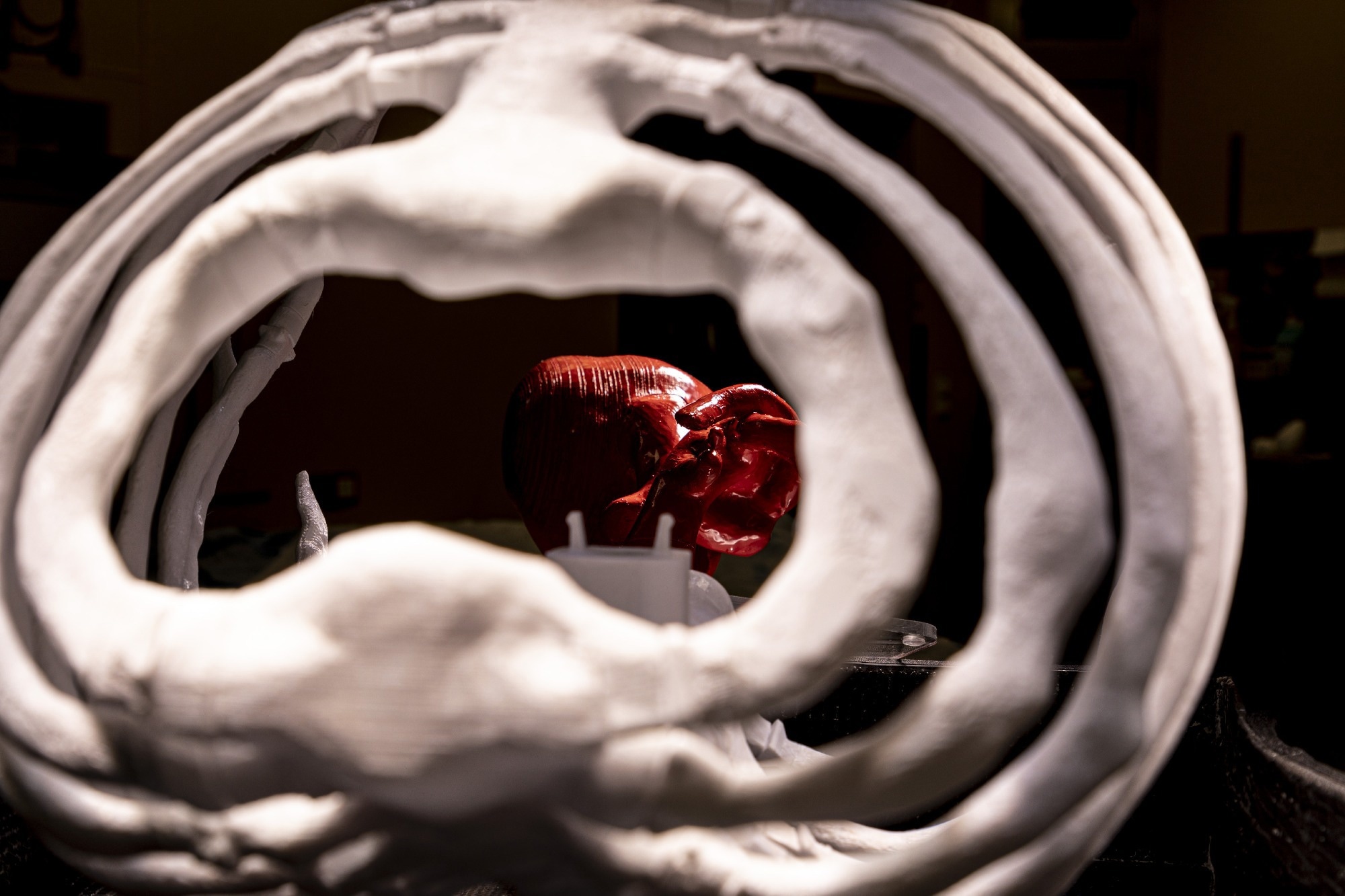
Image Credit: Magdeburg University Hospital
HW: Currently, for much surgical training, animals are used. If you come from the field of tissue engineering, you are experienced in creating alternatives to animal models that have the same functions. In our new development, we, therefore, implement this goal. First, we have a realistic copy of the human rib cage that the surgeons can train with, and secondly, we can insert bioartificial human tissues, for example, lung tumors.
For image-guided interventions, academia and industry are developing electrodes and other devices for thoracic operations. Many of these devices must be usable in the context of MRTs. Therefore we modified our materials so that you can use them under MRT.
With further ideas coming from our shareholders and our scientific partners, we continue to develop our product and our company. At MEDICA, our development already appealed to various representatives from academia and industry.
What are the materials used in the thorax models?
HW: We are really focusing on the material so that the model ribs have the physiological behavior of human ribs. That is why the industry can optimize their implants with it because they break and act exactly like human bones. For training purposes, it is much cheaper to work with one standard model, but if someone is interested in a patient-specific individualized thoracic model, it is possible to create one from CT data.

Image Credit: Magdeburg University Hospital
We have filed patents for the materials. The bony structures are generated from modified polymers. The bioartificial human tissues are based on collagen compounds.
Why is there a need for better models of the thorax specifically?
TW: In minimally invasive thoracic surgery operations, the patient is lying on their side. The anesthesiologist taking care of the patient will block the upper lung so it will deflate and collapse. As a result, a cavity forms between the chest wall and the collapsed lung. The surgeon goes inside this space with their instruments and does whatever they have to do to perform the operation. Sometimes, he has to flip the lung from the back to the front to reach the posterior side or the other way around.

Image Credit: Magdeburg University Hospital
The challenge is to do these operative maneuvers in the restricted space of the thoracic cavity. There are different training models to practice minimal invasive operations of the pelvis and abdomen; compared to the actual situation in the chest these models allow a large amount of freedom for performing the operations.
HW: We cover our training models with a soft tissue layer that we have developed so that you can't see inside. Trainee doctors really have to learn how to access the rib cage and train to feel the ribs. In order to create realistic operating conditions, animal organs can be placed in our training model, for example. The organs can also be perfused and ventilated.
What is the benefit of 3D printing the ribs?
HW: Our additive production approach enables the anatomically correct imitation of the anatomical structure of ribs by mapping the two cortical parts and the marrow cavity for the first time. In addition, a rib is not a harmoniously curved bone with an oval cross-section but changes its shape several times in the anatomical course.
Several healthcare companies that supply implants for rib re-fixation have tested our preliminary models and started to use them for training doctors and medical users on how to apply their implants.
After surgical or implant training, if a rib is broken, we can exchange it easily, and it can be broken again in another position if necessary.
How do these models help to reduce the need for animals in surgical training?
TW: The exact anatomical representation of the human thoracic skeleton provides a more realistic training environment than many established animal models. Fresh or commercially available animal organs can be used for a realistic depiction of the visceral surgical steps, but in any case, this model reduces the need for laboratory animals. No special premises are required for the use of our training models; in this way, a training stand can be made from any office or seminar work station.
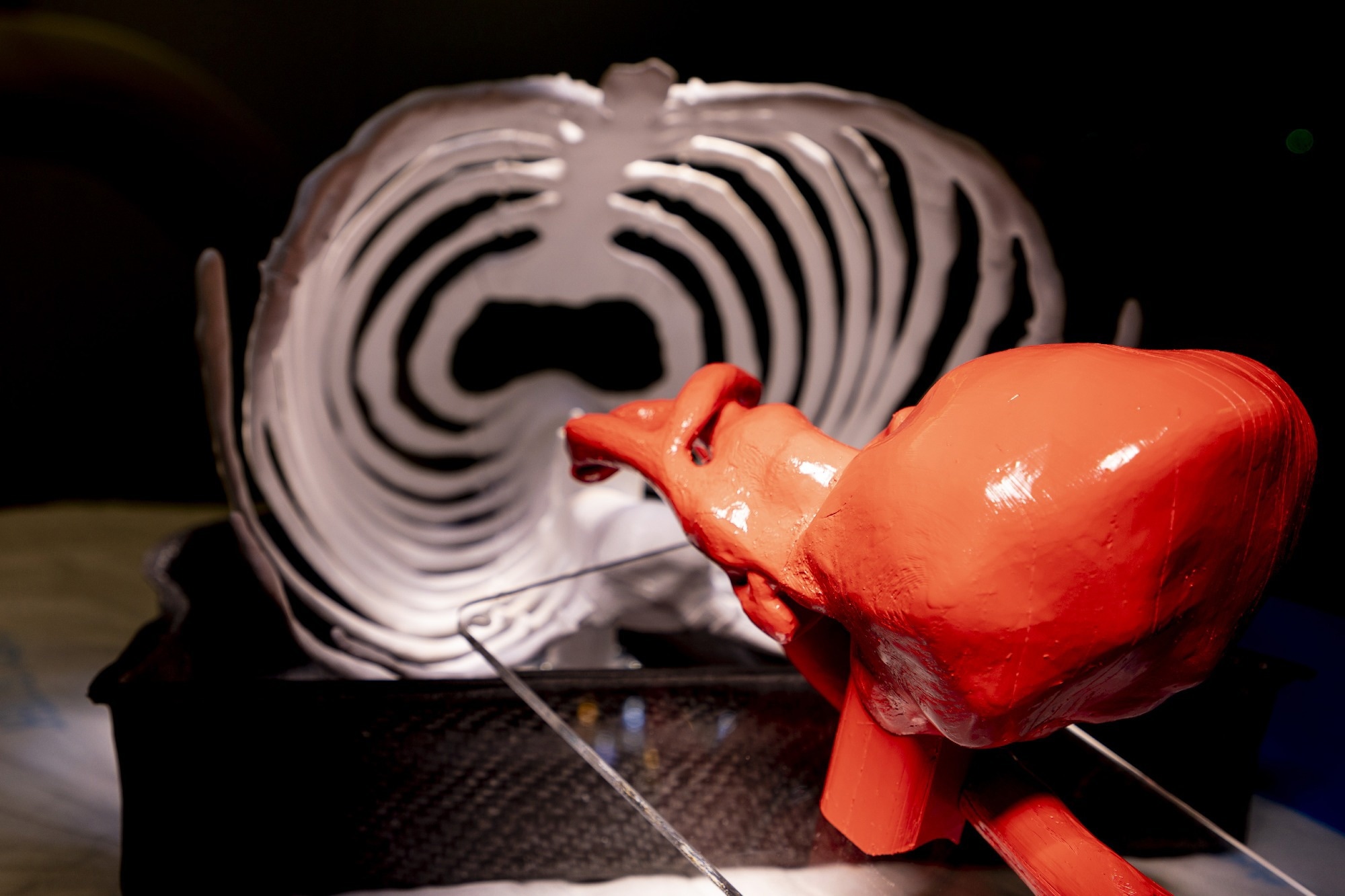
Image Credit: Magdeburg University Hospital
We started to use our model also for student training because every young doctor has to learn the insertion of a chest tube. Compared to the effort of having to get an animal carcass from the slaughterhouse, our model is much easier to organize and handle.
Why is it important for your models to show up in MRIs and CTs?
TW: This feature is not necessary for surgeons, but we have in mind that we could use our model for training interventional radiologists. For example, minimally invasive interventions on the chest, such as percutaneous nodule biopsy or radiofrequency ablations, can be trained for.
How important are trade shows like MEDICA to promote new innovations such as your own?
HW: For us as a small and young spin-off, it was really very important. We wanted to find out whether our development appeals to the user groups, and to do that I think it's very important to have ventures like this.

Image Credit: MD2B LifeScience
TW: We are still at the beginning of development and we can go in different directions. Being a small start-up we have to decide what makes more sense and what's the next step. At MEDICA we get feedback from professionals, potential future customers, or other academics. MEDICA helps us to develop a sense of what the market wants.
HW: It is really fantastic to discover that your idea is relevant.
Are there any clear immediate next steps you will be taking to improve upon your current models?
HW: We will focus on finalizing the soft tissue coverage. Next, we will have to implement models for the visceral organs in the thorax.
TW: Is it the chest and the rib cage itself that's interesting for most people? Or do we have to put in more effort to come up with an idea for the inner organs like the heart and lungs? Is it sufficient to take organs from slaughtered animals or do people need artificial organs made from silicon, plastics, etc? There are already products in the market, but we have the idea of depicting the haptics of organs to give the user a realistic experience during their training and interventions. So the question is: How close can we get with the artificial technologies that we have at hand right now?
About Heike Walles & Thorsten Walles
 Heike Walles, Ph.D. Born in 1962 in Germany. 1982 - 1988 Studied Biology at the Justus-Liebig-University Gießen,Germany. 1989 – 1994 PhD thesis at the Ludwig-Maximilians University in Munich1999 – 2003 Post-Doc and Junior-Professor at Leibniz-Research-Laboratories for Biotechnology and Artificial Organs (LEBAO), Hannover Medical School, Hannover. 2004 – 2012 Head of Department Cellsystems, Fraunhofer-Institute Interfacial Engineering and Biotechnology (IGB), Stuttgart. 2009 – 2018 Full-Professor for Tissue Engineering and Regenerative Medicine, Julius-Maximilians-University, Würzburg. 2014-2018 Head of Fraunhofer Translational Center for Regenerative Therapies in Oncology and Musculoskeletal Diseases, Würzburg. Since 2018 Head of Core-Facility Tissue-Engineering, Otto-von-Guericke-University, Magdeburg, Germany. 2011 Co-founder of the TissUse GmbH (Berlin). 2022 Co-founder of MD2B LifeSciences GmbH (Magdeburg).
Heike Walles, Ph.D. Born in 1962 in Germany. 1982 - 1988 Studied Biology at the Justus-Liebig-University Gießen,Germany. 1989 – 1994 PhD thesis at the Ludwig-Maximilians University in Munich1999 – 2003 Post-Doc and Junior-Professor at Leibniz-Research-Laboratories for Biotechnology and Artificial Organs (LEBAO), Hannover Medical School, Hannover. 2004 – 2012 Head of Department Cellsystems, Fraunhofer-Institute Interfacial Engineering and Biotechnology (IGB), Stuttgart. 2009 – 2018 Full-Professor for Tissue Engineering and Regenerative Medicine, Julius-Maximilians-University, Würzburg. 2014-2018 Head of Fraunhofer Translational Center for Regenerative Therapies in Oncology and Musculoskeletal Diseases, Würzburg. Since 2018 Head of Core-Facility Tissue-Engineering, Otto-von-Guericke-University, Magdeburg, Germany. 2011 Co-founder of the TissUse GmbH (Berlin). 2022 Co-founder of MD2B LifeSciences GmbH (Magdeburg).
Thorsten Walles, MD FETCS. Born in 1972 in Germany. 1993-2000 Studied medicine at the Hanover Medical School. 1997-1998 Research stay at the Johns Hopkins University (Baltimore, USA). 2000-2009 Clinical training in cardiac, thoracic and vascular surgery as well general surgery. 2009 specialist in thoracic surgery. Since 2017 professor for Thoracic Surgery and chief of the Thoracic Surgery Service at the University Hospital Magdeburg. Focus: oncological surgery, minimally invasive thoracic surgery including robot-assisted surgery, pediatric thoracic surgery, thoracic traumatology. 2011 Co-founder of the TissUse Gmbh (Berlin). 2022 Co-founder of MD2B LifeSciences GmbH (Magdeburg).