Sponsored Content by IpsenReviewed by Olivia FrostDec 15 2022
Over 400,000 people are diagnosed with renal cell carcinoma (RCC) globally each year,i and as innovations in treatment have resulted in helping people live longer and better than ever before, their experiences and preferences are an important part of their journey. In this interview, we speak to Steve Pointon, patient advocate in remission from RCC and Dr Harm van Melick, Consultant Urologist, about their experiences with shared decision making and the impact it can have on people living with RCC.
Please could you introduce yourselves and explain your background or experience with renal cell carcinoma
Steve Pointon: I am a patient advocate and qualified counsellor working with a national kidney cancer support network. Whilst training to become a counsellor, I volunteered in a local hospice, and now I run my own counselling business and work for a social enterprise. After being diagnosed with RCC, going into remission and then finding out the cancer had returned, all in the space of 18 months, I have now been in remission since 2018 and I remain dedicated to helping others through their cancer diagnosis and treatment journeys.
Dr Harm van Melick: I have been a consultant urologist for over a decade, and currently work at St. Antonius Hospital in Nieuwegein and Utrecht, the Netherlands. My specialist interests are in uro-oncology, robotic and laparoscopic surgery, and image guided diagnostics. During my career I have worked to develop and implement shared decision making tools to support patients through their treatments.
Shared decision making has been a growing part of the kidney cancer treatment pathway over the last 10 years. What is it, and how does it benefit people living with RCC?
Steve: When I was first diagnosed with RCC, the loss of control over my future was huge. I believe anything we can do to bring people into the treatment conversation after diagnosis is key to helping them feel in control. Shared decision making is about having open communication with your healthcare provider and being included and informed throughout your treatment. Even if there is only one treatment option available, a shared decision making approach means that you’re able to understand what’s happening to your body and you can feel empowered with that knowledge.
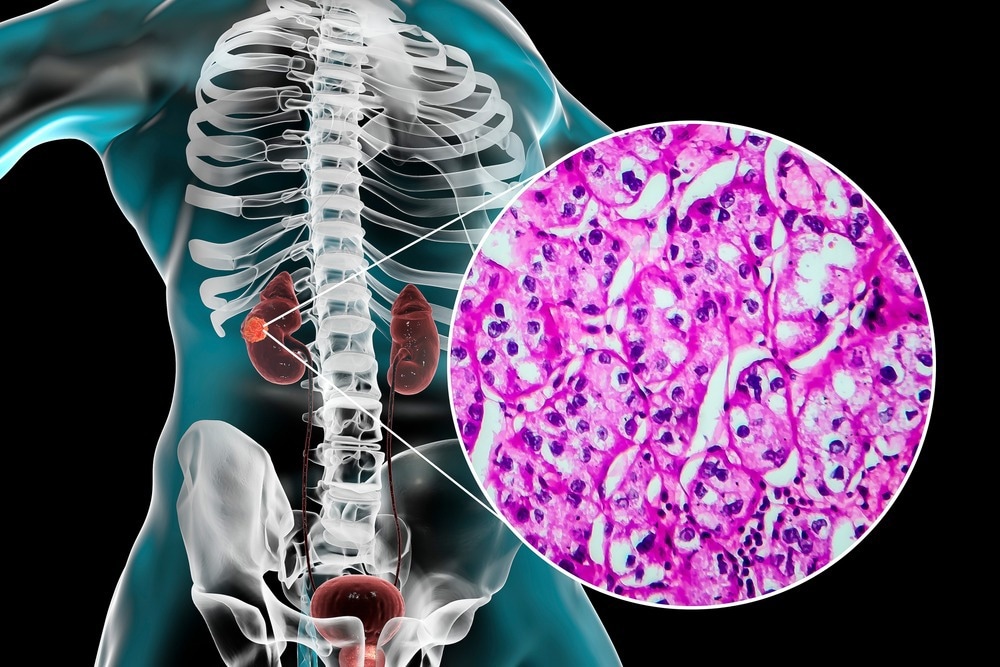
Image Credit: ShutterStock/Kateryna Kon
Dr van Melick: We’ve seen a significant change in RCC treatment options and care pathways over the last decade, which alters how we must approach RCC care. Simply put, shared decision making is an approach where healthcare providers give the best information possible to their patients so that people living with an RCC diagnosis can consider their own values and preferences when choosing the best treatments for them. The difference is the emphasis on open communication.
The traditional method of simply telling a patient that they must do something based primarily on clinical evidence and outcomes does not account for their needs and wishes as a person living with the disease. Different treatment options can impact a person’s life in a variety of ways, and we should not make the ultimate decisions for them. Shared decision making still includes healthcare providers as experts to help inform, educate and make sense of the complex management of the disease. However, people living with RCC are experts on their own bodies and disease experiences – it’s important that we remember that.
Steve, what did a shared decision making approach look like in practice during your treatment?
Steve: When I found out the RCC had returned following my initial remission, I went through the motions of diagnosis and treatment planning for a second time. I was told all the treatment options available, which one my physician recommended, and what the likely side effects would be. The choice was then in my hands. I had young children at the time, and I wanted to do everything possible to be here and see them grow up.
Even after I began treatment, my healthcare team made it clear that I could choose to stop at any time. Through conversations with my physician and listening to their expert knowledge, I felt I had an ultimate say over my care. Now I look back at my treatment, I don’t have any doubt or regret over my experience because it was my choice.
What are the benefits of shared decision making over traditional consultations?
Dr van Melick: We first see shared decision making discussed in academic literature in the 1990s, and it has increased over time. The evidence shows a number of benefits: less decisional regret,ii higher rates of treatment compliance,iii higher levels of satisfaction with treatment,iv people are more involved and better informed,iii patients’ goals are achieved. You also see a decrease in the number of surgical interventions,v practice variation is going downvi and there is a reduction in overall cost.vii
Most importantly, though, choosing their own options lets people living with RCC decide the quality of life they want during treatment.
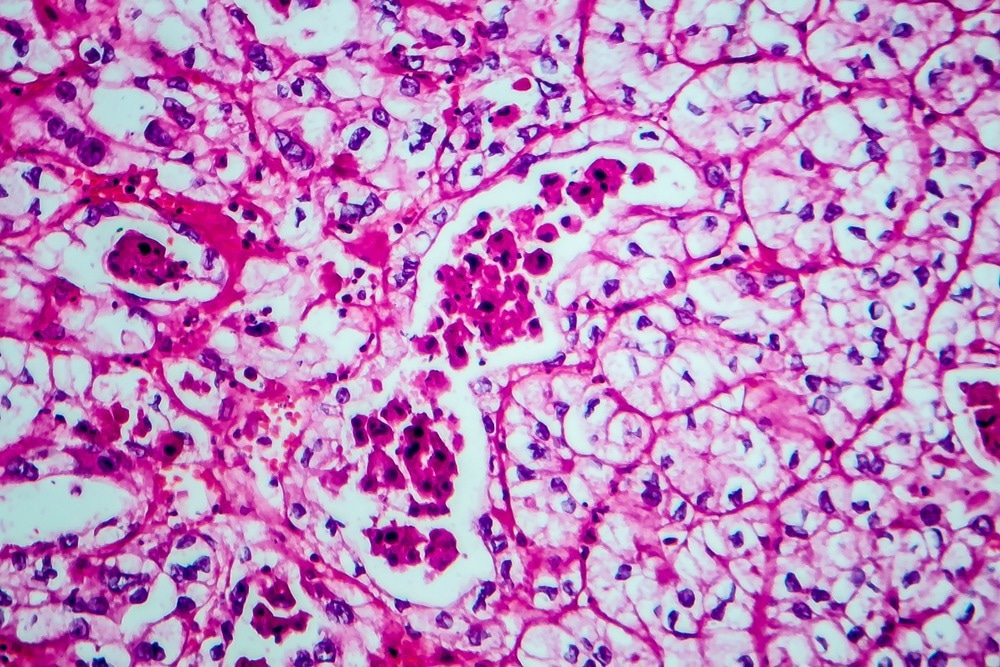
Image Credit: ShutterStock/Kateryna Kon
Steve: It’s really the quality-of-life consideration that has to be done together. When living with RCC, I feel the impact of the treatment decisions every day of my life. While my healthcare team was supportive and highly educated, they didn’t have the same perspective and lived experience to truly understand what I was going through.
This is where patient support groups and connecting with other people makes a difference during the shared decision making process. When I connected with my local group, I discovered new things about living with RCC and the journey I was going through. I could discuss the things I learned with my physician, with the reassurance that I would be listened to.
What should healthcare providers consider when adopting a shared decision making consultation process?
Dr van Melick: As healthcare providers, we come from a clinical research background that someone who is diagnosed with RCC will not have. Our task is to use clear and simple language to explain the complex treatment options, avoiding medical jargon, provide support in evaluating their decisions without any personal bias towards certain medications, and to repeat information as often as possible to help our patient understand.
This process should involve the whole integrated care team, such as specialist nurses, to improve communication with the patient and help with sensitive matters, when needed.
Steve: I would ask that healthcare providers be open to listening when someone comes to them to discuss treatment. You may provide this treatment all the time, but your patient might have heard of other options they would like to explore. Unfortunately, some healthcare providers can be resistant and aren’t always open to these discussions and that can be upsetting or frustrating when your life is so impacted by it.

Image Credit: ShutterStock/Ground Picture
Where do we go from here?
Dr van Melick: Clinically, most shared decision making guidelines relate to cancer in general. For example, neither the European Society for Medical Oncology guidelines nor the European Association of Urology guidelines include specific recommendations for RCC, although the latter includes it for prostate cancer. Only the American Society of Clinical Oncology highlights shared decision making as the recommended approach in RCC.
We’ve seen important work done by groups like the International Kidney Cancer Coalition (IKCC) through the creation of decision aids and workshops. Given the dynamic nature of RCC treatment, the innovations in the space and potential variation across regions, I hope to see a shared decision aid tool developed that would increase standardisation of practice and better support healthcare providers, especially in the face of new approaches.
Steve: We need people living with an RCC diagnosis to feel empowered and in control of their treatment journey as much as possible. Local patient support groups should have access to information and tools that work for their communities. I hope to see shared decision making become an increasingly normal experience for people living with RCC.
Cancer can take a lot of control away from you, so why wouldn’t we want to give some of it back if we could?
References
- Padala, Sandeep Anand et al. Epidemiology of Renal Cell Carcinoma. World Journal of Oncology, (11)3. 2020. 79-87. doi:10.14740/wjon1279
- Chichua, Mariam et al. Shared decision‑making and the lessons learned about decision regret in cancer patients. Supportive Care in Cancer, 30. 2022. 4587–4590. doi:10.1007/s00520-021-06725-5
- Fiorillo, A. et al. The role of shared decision‑making in improving adherence to pharmacological treatments in patients with schizophrenia: a clinical review. Annals of General Psychiatry, (19)43. 2020. doi:10.1186/s12991-020-00293-4
- Paduca, A. et al. Shared decision making and patients satisfaction with strabismus care—a pilot study. BMC Medical Informatics and Decision Making, (21)109. 2021. doi:10.1186/s12911-021-01469-y
- Niburski, K. et al. Shared decision making in surgery: A scoping review of the literature. Health Expectations, (23). 2020. 1241–1249. doi:10.1111/hex.13105
- NHS England. Why is shared decision making important? 2022. Date accessed November 2022. Available at: https://www.england.nhs.uk/personalisedcare/shared-decision-making/why-is-shared-decision-making-important/
- Coulter, A. & Collins, A. Making Shared Decision-Making a Reality: No decision about me, without me. The Kings Fund, 2011. Date accessed November 2022. Available at: https://www.kingsfund.org.uk/sites/default/files/Making-shared-decision-making-a-reality-paper-Angela-Coulter-Alf-Collins-July-2011_0.pdf
November 2022 | ALLSC-ALL-000890
About Ipsen
Ipsen is a global, mid-sized biopharmaceutical company focused on transformative medicines in Oncology, Rare Disease and Neuroscience. With Specialty Care sales of €2.6bn in FY 2021, Ipsen sells medicines in over 100 countries. Alongside its external-innovation strategy, the Company’s research and development efforts are focused on its innovative and differentiated technological platforms located in the heart of leading biotechnological and life-science hubs: Paris-Saclay, France; Oxford, U.K.; Cambridge, U.S.; Shanghai, China. Ipsen, excluding its Consumer HealthCare business, has around 4,500 colleagues worldwide and is listed in Paris (Euronext: IPN) and in the U.S. through a Sponsored Level I American Depositary Receipt program (ADR: IPSEY).