In a recent study published in the journal Nature Medicine, a group of researchers assessed if a precise blood test matches or surpasses traditional cerebrospinal fluid (CSF) tests in detecting Alzheimer's disease (AD) pathology, utilizing the BioFINDER-2 and Knight Alzheimer Disease Research Center (ADRC) cohorts.
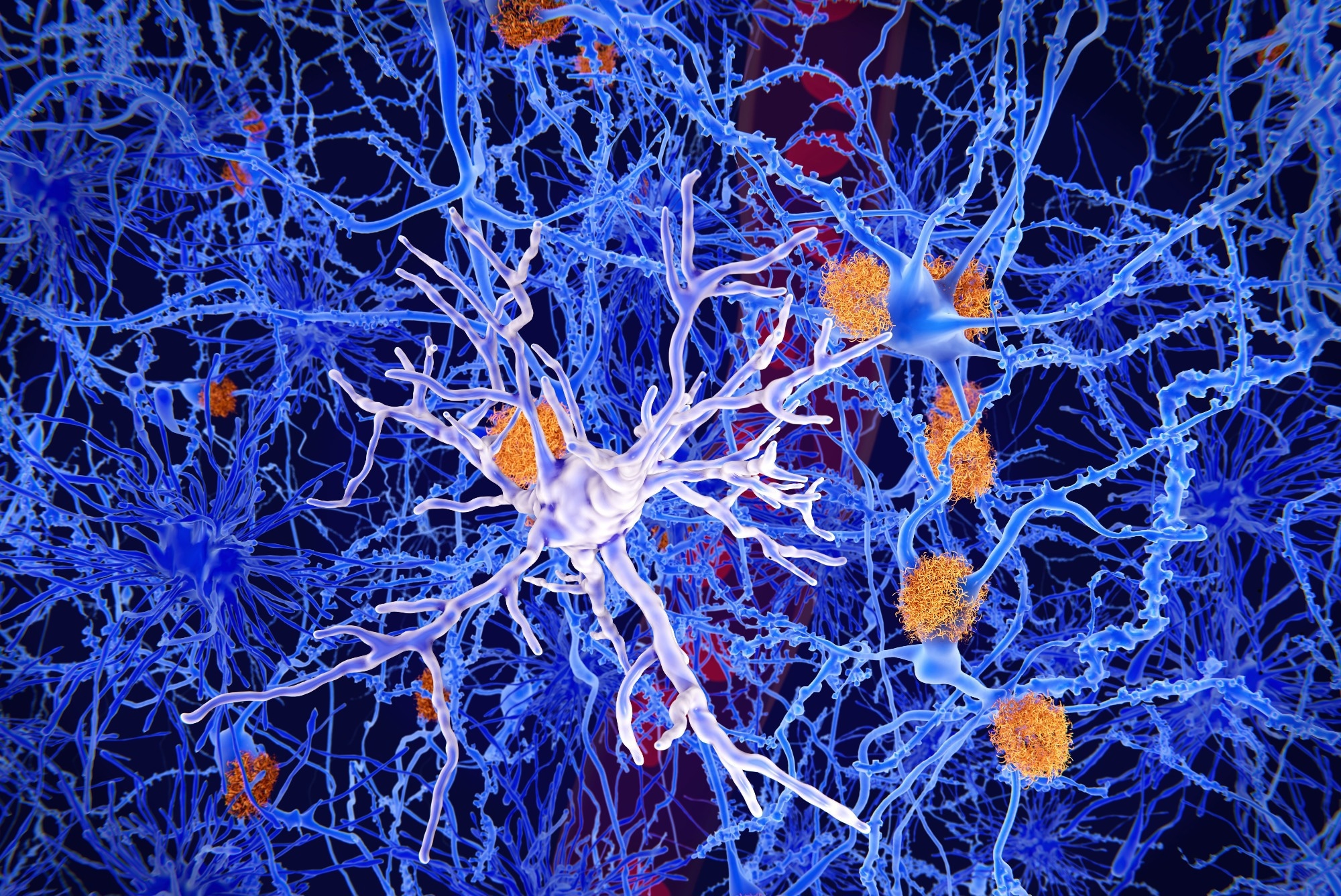 Study: Highly Accurate Blood Test for Alzheimer’s Disease Comparable or Superior to Clinical CSF Tests. Image Credit: Juan Gaertner / Shutterstock
Study: Highly Accurate Blood Test for Alzheimer’s Disease Comparable or Superior to Clinical CSF Tests. Image Credit: Juan Gaertner / Shutterstock
Background
Dementia, impacting over 40 million people worldwide with projections to rise to 130 million by 2050, leads to an annual global cost of about USD 1 trillion. AD, accounting for 60-70% of dementia cases, features the accumulation of amyloid-β (Aβ) plaques and tau tangles, key markers of the disease. These biomarkers are associated with the disease's progression, from pre-symptomatic stages to cognitive decline. Recent advancements, such as the Food and Drug Administration (FDA)-approved lecanemab for early AD stages, highlight the importance of detecting Aβ pathology, traditionally done through positron emission tomography (PET) scans or CSF assays. However, their high costs and invasiveness limit widespread use, prompting interest in blood-based markers like plasma phosphorylated tau (p-tau), especially p-tau217, for their potential in AD pathology detection. Despite their promise, the standalone diagnostic utility of these markers is yet to be fully endorsed, underlining the need for further research to establish their efficacy and reliability across various populations and disease stages.
About the study
The present study incorporated participants from two distinct observational cohorts: BioFINDER-2 from Sweden and the Knight ADRC in the United States (US). BioFINDER-2 involved participants from Swedish medical facilities, encompassing both cognitively unimpaired individuals and those with various stages of cognitive impairment, including mild cognitive impairment (MCI), AD dementia, and other neurodegenerative diseases. The classification of MCI and AD dementia followed established criteria based on cognitive performance and the presence of Aβ pathology. The Knight ADRC cohort, focusing on memory and aging research, included participants from the St. Louis area assessed for cognitive impairment and AD-related clinical syndromes. Both cohorts required participants to undergo Aβ and tau PET scans and have available plasma for analysis.
CSF biomarkers were analyzed using both cohorts' FDA-approved and clinically validated assays for Aβ and tau proteins, adhering to international collection and handling standards. Blood samples were collected concurrently with CSF to measure p-tau217 through mass spectrometry, calculating the ratio to non-phosphorylated tau.
Imaging outcomes utilized approved PET tracers to measure amyloid and tau pathology, with standardized uptake value ratios (SUVR) and Centiloids facilitating comparison across tracers and studies. Statistical analyses evaluated the diagnostic capabilities of plasma %p-tau217, which measures the ratio of phosphorylated-tau217 to non-phosphorylated tau in comparison to CSF biomarkers. They utilized receiver operating characteristic (ROC) curves and additional metrics to determine the accuracy and predictive value, while sensitivity analyses reinforced the reliability of the results.
Study results
The BioFINDER-2 study from Sweden included 1,422 participants, with a near-even split between cognitively impaired and unimpaired individuals, while the Knight ADRC cohort from the US comprised 337 participants, with a smaller proportion identified as cognitively impaired. The analysis employed area under the curve (AUC) metrics for comparing the diagnostic performance of %p-tau217 against traditional CSF biomarkers
In terms of Aβ PET status classification across both cohorts, %p-tau217 demonstrated high diagnostic accuracy, showing equivalence to or surpassing that of CSF biomarkers. Specifically, in the BioFINDER-2 cohort, %p-tau217 achieved an AUC of 0.97, comparable to CSF Elecsys p-tau181/Aβ42 and Aβ42/40 ratios. Similar outcomes were observed in the Knight ADRC cohort, underscoring the potential of plasma %p-tau217 as a viable alternative for Aβ pathology detection.
Further analysis focused on cognitively impaired participants, highlighting the clinical relevance of %p-tau217 in identifying candidates for anti-Aβ immunotherapies. In these groups, %p-tau217 predicted Aβ PET status with high overall accuracy and positive and negative predictive values, aligning closely with the performance metrics of established CSF biomarkers. This finding suggests the equivalence of plasma and CSF biomarkers in diagnosing Aβ pathology among cognitively impaired individuals.
The study also explored the diagnostic accuracy of %p-tau217 for tau PET status, revealing superior performance compared to CSF biomarkers in the BioFINDER-2 cohort. This superiority was further validated in the Knight ADRC cohort, emphasizing %p-tau217's effectiveness in tau pathology detection. A novel two-cut-off approach was applied, further enhancing diagnostic accuracy by categorizing results into clear, abnormal, and intermediate values, demonstrating % p-tau217's robustness in predicting AD pathology.
Sensitivity analyses confirmed the reliability of plasma %p-tau217 as a diagnostic tool, showing consistent results across different cohorts and methodologies. Notably, a longitudinal sub-study within the Knight ADRC cohort confirmed the stability of %p-tau217 levels over time, underscoring its reliability for repeated measures. This comprehensive evaluation highlights plasma %p-tau217's clinical equivalence to traditional biomarkers, offering a less invasive, equally accurate alternative for AD diagnosis.