In a recent study published in the journal Frontiers in Endocrinology, researchers examined how lifestyle factors and fertility-specific quality of life (QOL) influence the outcomes of assisted reproductive technology (ART) treatments.
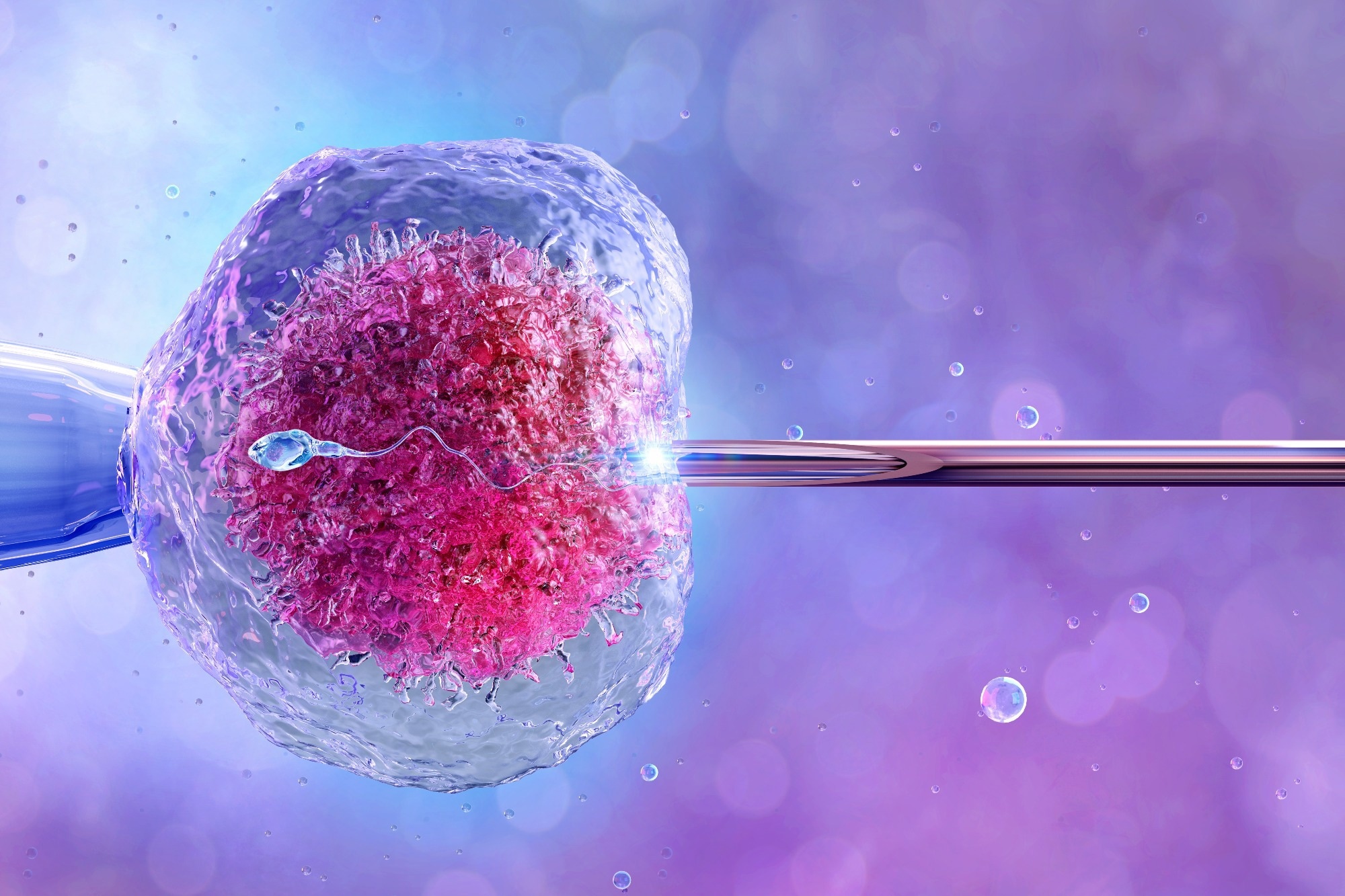 Study: Lifestyle and fertility-specific quality of life affect reproductive outcomes in couples undergoing in vitro fertilization. Image Credit: Corona Borealis Studio / Shutterstock
Study: Lifestyle and fertility-specific quality of life affect reproductive outcomes in couples undergoing in vitro fertilization. Image Credit: Corona Borealis Studio / Shutterstock
Background
Infertility impacts around 48.5 million couples worldwide, leading to an increase in ART treatments, with 2.5-3 million cycles annually and nearly 450,000 in Japan alone. With 1 in every 13.9 Japanese babies born via ART, the influence of factors like age, ovarian reserve, and lifestyle choices- including diet, smoking, exercise, and sleep- on treatment success is recognized. The World Health Organization (WHO) highlights the need to assess QOL, including fertility-specific QOL, via tools like the Fertility Quality of Life tool (FertiQoL). The relationship between fertility-specific QOL and ART outcomes, however, requires further research to understand their complex interactions better.
About the study
The present study focused on infertile couples undergoing their first in vitro fertilization (IVF) treatment in Japan, selecting participants based on specific health and demographic criteria. At the outset, participants detailed their dietary habits, modeled after the Mediterranean diet but tailored to Japanese preferences, and lifestyle choices, including sleep patterns, work habits, computer usage, smoking status, and physical activity, measured by metabolic equivalent tasks (METs). Additionally, the fertility-specific quality of life was assessed using the Japanese version of the FertiQoL questionnaire, exploring its influence on treatment outcomes.
The study outlined the protocols for controlled ovarian stimulation, laboratory procedures, and embryo transfer (ET), including medication dosages and administration schedules based on individual patient profiles. The selection of good-quality blastocysts for transfer was based on the Gardner classification, with a wash-out period required between stimulation and ET. Outcomes of the IVF/intracytoplasmic sperm injection (ICSI) were precisely recorded, from hormone levels to the rates of fertilization, embryo development, and pregnancy confirmation via serum Human Chorionic Gonadotropin (hCG) test and transvaginal ultrasound for gestational sac (GS) detection.
Statistical analysis aimed to explore the relationship between patient background, dietary and exercise habits, FertiQoL scores, and IVF outcomes, using a multivariable approach to identify significant factors. The study attempted to recruit 286 patients to detect a clinically relevant difference in the primary outcome, the good-quality blastocyst rate, with comprehensive statistical analysis performed using SAS software.
Study results
Between May 2019 and March 2022, 291 women seeking their first IVF treatment at clinics within the IVF Japan Group and the University of Tokyo Hospital were initially considered for the study. After excluding those who discontinued treatment, became pregnant spontaneously, or met exclusion criteria, 281 women proceeded with controlled ovarian stimulation and oocyte retrieval. Various reasons, including lack of fertilization, absence of good-quality embryos, and loss of follow-up, further narrowed the participants to 260 who underwent ET, with 200 undergoing single blastocyst embryo transfers (blast-SETs). Of these, 139 women showed positive hCG levels, indicating pregnancy, and in 121 women, a single GS was detected without instances of multiple GSs.
The study examined the rate of good-quality blastocysts per oocyte retrieval, revealing that women over 36 years old or those with Hashimoto's disease had significantly lower rates, while frequent fish consumption was also tentatively linked to lower rates. Analysis of all ET cycles showed that older women had lower chances of a positive pregnancy test. In contrast, adequate sleep, computer use, and non-smoking partners were associated with higher chances. GS detection post-ET was more likely with the use of olive oil, more prolonged computer use, and a body mass index (BMI) of 20.8 kg/m2 or higher, with older age decreasing the likelihood.
Explicitly focusing on blast-SET cycles, computer use for four or more hours a day significantly improved the chances of a positive pregnancy test and GS detection. Older age tended to decrease the likelihood of a positive pregnancy test, while a higher FertiQoL Total scaled treatment score and a certain BMI threshold appeared to favor GS detection, however, with a trend towards significance rather than definitive proof.
Conclusions
To summarize, the study explored the effects of lifestyle, dietary habits, and fertility-specific QoL on ART outcomes among Eastern Asian women. Key findings include the negative impacts of advanced age and Hashimoto's disease on blastocyst quality and positive associations between adequate sleep, computer use, and pregnancy success. Olive oil consumption emerged as beneficial for gestational sac detection, challenging assumptions about dietary impacts on fertility. Notably, male smoking negatively affected outcomes, highlighting the importance of lifestyle factors in reproductive success.