In a recent study published in the JAMA Network Open, a group of researchers evaluated the impact of exercise, glucagon-like peptide-1 receptor agonist (GLP-1 RA) liraglutide, and their combination on bone health at the hip, spine, and forearm following diet-induced weight loss in adults with obesity.
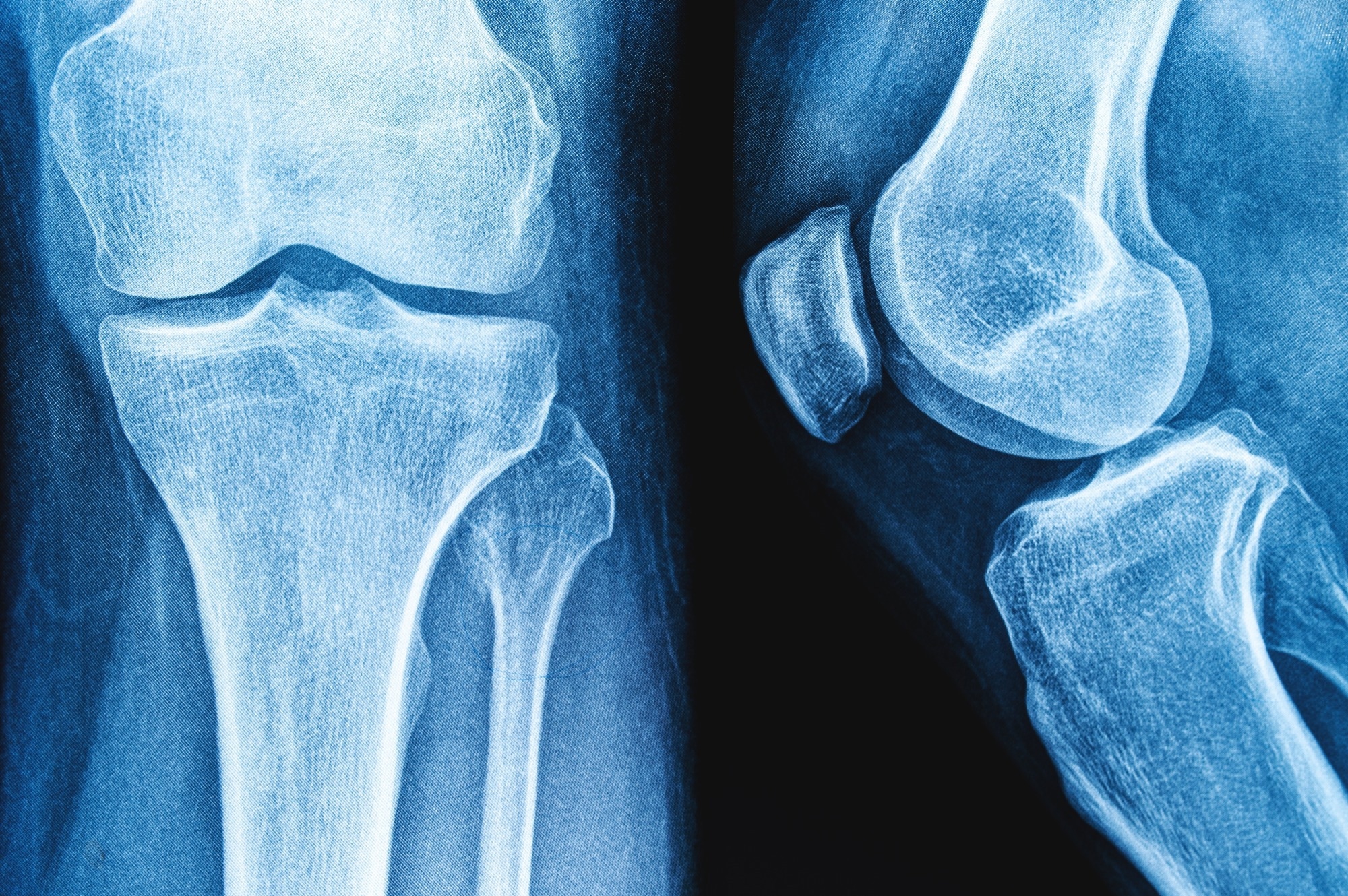 Study: Bone Health After Exercise Alone, GLP-1 Receptor Agonist Treatment, or Combination Treatment. Image Credit: siamionau pavel / Shutterstock
Study: Bone Health After Exercise Alone, GLP-1 Receptor Agonist Treatment, or Combination Treatment. Image Credit: siamionau pavel / Shutterstock
Background
Weight loss reduces obesity-related comorbidities but often leads to decreased bone mineral density (BMD) and increased bone turnover, raising fracture risk and mortality. This bone loss is a concern across the lifespan, particularly in older adults, and is observed after gastric bypass and calorie restriction. Identifying treatments that induce weight loss while minimizing bone loss is crucial. GLP-1RAs promote weight loss by suppressing appetite. Exercise is recommended for healthy weight loss as it preserves lean mass. Further research is needed to establish the long-term effects of GLP-1 RAs and exercise on bone health following significant weight loss, as current evidence is limited and inconsistent.
About the study
The present study was conducted from August 2016 to November 2019 at Hvidovre Hospital and the University of Copenhagen. It was approved by the Regional Ethics Committee in Denmark and the Danish Medicines Agency, following Consolidated Standards of Reporting Trials (CONSORT) guidelines. Participants aged 18-65 with a body mass index (BMI) of 32-43 provided informed consent. Those with serious chronic illnesses, including diabetes, were excluded. After an 8-week low-calorie diet (800 kcal/day), participants who lost at least 5% of their initial body weight were randomized into four groups: exercise and placebo, liraglutide, a combination of exercise and liraglutide, or placebo.
The exercise intervention included a 6-week ramp-up phase, followed by vigorous-intensity group and individual sessions. Liraglutide or placebo was administered daily, starting at 0.6 mg and increasing to 3.0 mg or the highest tolerated dose. Monthly weight consultations with dietetic support were provided.
Outcomes included body weight, composition, and BMD at the hip, lumbar spine, and forearm, measured by dual-energy x-ray absorptiometry (DXA). Bone turnover markers, plasma type 1 collagen cross-linked C-telopeptide (P-CTX), and plasma propeptide of type 1 procollagen (P-P1NP) were assessed from fasting blood samples. The statistical analysis used constrained linear mixed models, adjusting for baseline measurements, with a two-sided P < .05 considered significant. Data analysis occurred from March to April 2023, with additional analysis in February 2024.
Study results
A total of 195 participants (mean age 42.84 years; 64% female; mean BMI 37.00) completed the low-calorie diet and were randomized into four groups: exercise (48 participants), liraglutide (49 participants), combination (49 participants), and placebo (49 participants). BMD measurements were available for 158 to 161 participants at week 52. No participants were on osteoporosis medications, and no fragility fractures occurred. Safety outcomes were reported previously.
The mean exercise volume was 118 minutes/week at 78% of maximum heart rate in the exercise group and 111 minutes/week at 79% in the combination group. Eight participants completed the study on a lower medication dose, and 11 discontinued the study medication but remained in the study.
The estimated mean weight loss was 7.03 kg in the placebo group, 11.19 kg in the exercise group, 13.74 kg in the liraglutide group, and 16.88 kg in the combination group. After the initial weight loss of 13.1 kg, the placebo group regained weight, while the exercise and liraglutide groups maintained their weight loss, and the combination group lost additional weight. Both the exercise and liraglutide groups reduced fat percentage and mass, with the combination group showing the greatest reductions. The exercise group increased lean mass, and the combination group preserved lean mass despite significant fat loss.
Changes in BMD from before the low-calorie diet to week 52 showed that the combination group had no significant changes in BMD compared to the placebo at the hip and lumbar spine. However, the liraglutide group experienced a decrease in hip and lumbar spine BMD compared to the exercise and placebo groups. The distal forearm BMD increased in the exercise and combination groups, with no significant differences between the four groups. Subgroup analyses by sex and age showed consistent results. Liraglutide and combination treatments were associated with increased whole-body BMD compared to placebo.
Bone turnover markers showed that P-CTX increased by 27% after the low-calorie diet and decreased in all groups by week 26, with the lowest levels in the placebo group. P-P1NP increased by 7% during the low-calorie diet and returned to initial levels by week 52 in all groups.
Conclusions
To summarize, this secondary analysis of a randomized clinical trial examined changes in site-specific BMD during diet-induced weight loss followed by a 1-year intervention with liraglutide (3.0 mg/day), exercise, or their combination, compared to placebo. The combination treatment led to the greatest weight and fat reduction while preserving BMD at the hip, spine, and forearm. Liraglutide alone reduced hip and spine BMD despite weight loss. Exercise alone maintained lean mass and preserved hip and spine BMD. The findings suggest that combining exercise with GLP-1RA therapy is the most effective strategy for weight loss while preserving bone health.