Background
Tumor-expressed mutant proteins that can be recognized by the immune system, called cancer neoantigens, are promising targets for immunotherapy. Advances in cancer sequencing and bioinformatics have enabled the identification of these neoantigens, leading to the development of vaccines that stimulate neoantigen-specific T-cell responses and antitumor immunity. Initial studies demonstrated the efficacy of neoantigen vaccines in preclinical models and human melanoma using various platforms, including dendritic cells, synthetic long peptide (SLP), and ribonucleic acid (RNA) vaccines. While these approaches have shown promise, the DNA vaccine platform offers unique advantages, including design flexibility, lower cost, and the ability to include multiple neoantigens in a single construct.
Neoantigen vaccines have also been evaluated in glioblastoma, pancreatic cancer, and other malignancies, proving safe and immunogenic in early trials. TNBC lacks targeted therapies and is associated with a high mutational burden and abundant tumor-infiltrating lymphocytes (TILs), which correlate with better outcomes. These features make TNBC an ideal candidate for neoantigen vaccine therapy. Despite this potential, no neoantigen DNA vaccine studies had been reported in breast cancer until this study. In the present study, researchers developed a neoantigen DNA vaccine platform enhanced with electroporation for improved immunogenicity. They investigated its effects via a phase 1 clinical trial in patients with persistent TNBC after chemotherapy.
About the Study
A total of 35 patients with persistent TNBC following neoadjuvant chemotherapy and without metastatic cancer or autoimmune disorders were enrolled between 2015 and 2018. Tumor biopsies and matched peripheral blood mononuclear cells (PBMCs) were collected for tumor-normal exome sequencing to detect somatic mutations and neoantigens. Neoantigens were identified using the pVACtools pipeline, which prioritized peptides based on binding affinity, expression, and mutation characteristics. DNA vaccines were designed to target prioritized neoantigens, incorporating a mutant ubiquitin sequence to enhance antigen presentation. Human leukocyte antigen (HLA) typing and validation assays ensured precise epitope targeting. Each vaccine underwent rigorous quality control, ensuring sterility and expression capability.
Seventeen subjects were excluded from treatment due to complete pathologic response, ductal carcinoma in situ, insufficient tumor tissue, patient preference, or disease recurrence. Eighteen patients received the vaccine, targeting a median of 10 neoantigens (4–20) after completing standard adjuvant therapy. The vaccine (4 mg) was administered intramuscularly using the TriGrid electroporation device on days 1, 29, and 57. To measure T-cell responses, peripheral blood was drawn for immunological assessments, including ELISpot and flow cytometry. Safety monitoring included clinical and laboratory evaluations. Toxicity was graded per the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE). Immune responses were confirmed using enzyme-linked immunosorbent spot assay, flow cytometry, and tetramer staining, followed by T-cell receptor (TCR) sequencing and clonotype analysis. Statistical analysis involved the use of Student’s t-test, Kaplan–Meier product-limit method, and log-rank test.
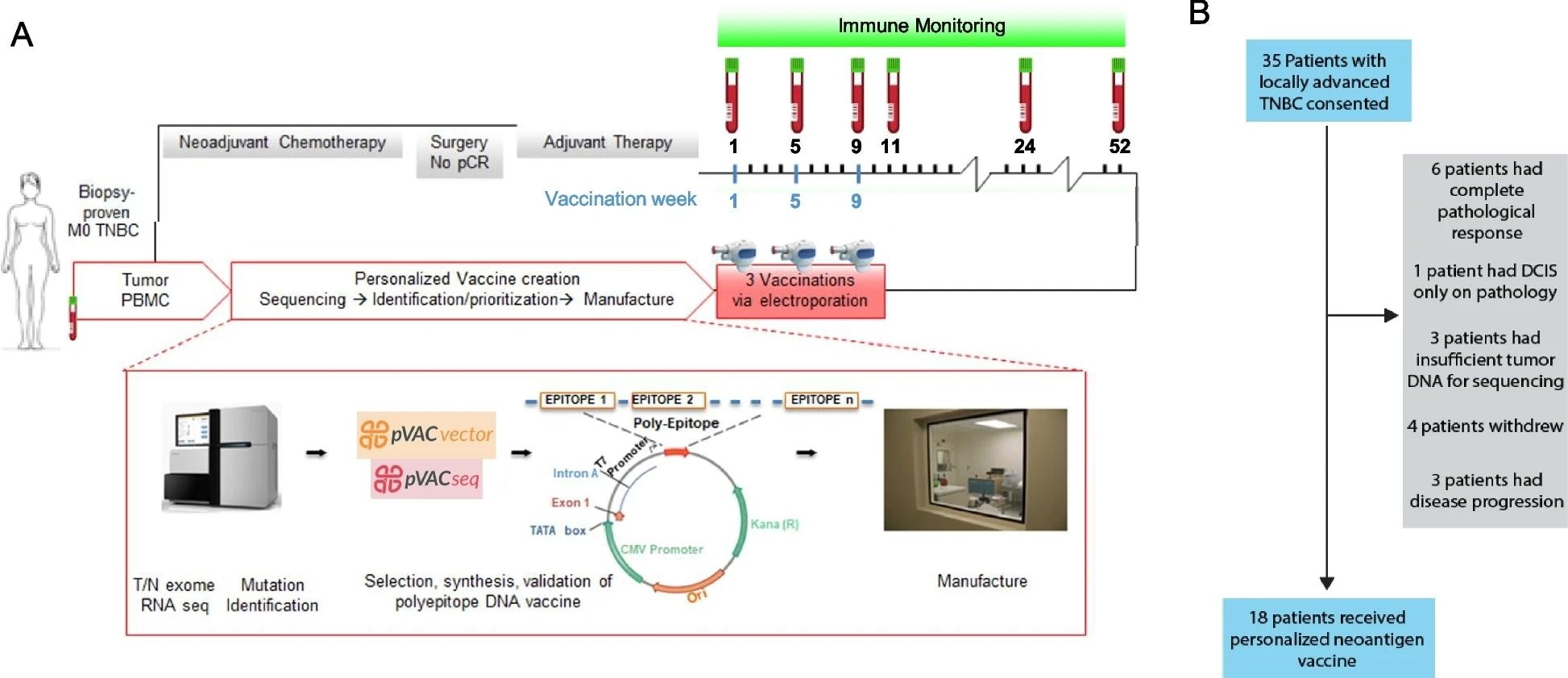 Design, manufacture, and administration of neoantigen DNA vaccines for TNBC patients. A Somatic mutations were identified by whole exome sequencing of tumor and germline DNA. Mutation expression was confirmed by tumor RNA-seq with cDNA capture. Candidate neoantigens were prioritized for inclusion in the vaccines on the basis of HLA binding predictions by pVAC-seq (Methods). Neoantigen DNA vaccines were administered intramuscularly using a TriGrid electroporation device. Peripheral blood was drawn prior at each vaccination timepoint and at selected timepoints after all vaccinations as indicated in A. B 35 patients with locally advanced TNBC were consented. Patients were excluded due to complete pathological response after neoadjuvant chemotherapy (NAC), insufficient tumor, patient withdrawal, and disease recurrence. 18 patients received personalized neoantigen DNA vaccines
Design, manufacture, and administration of neoantigen DNA vaccines for TNBC patients. A Somatic mutations were identified by whole exome sequencing of tumor and germline DNA. Mutation expression was confirmed by tumor RNA-seq with cDNA capture. Candidate neoantigens were prioritized for inclusion in the vaccines on the basis of HLA binding predictions by pVAC-seq (Methods). Neoantigen DNA vaccines were administered intramuscularly using a TriGrid electroporation device. Peripheral blood was drawn prior at each vaccination timepoint and at selected timepoints after all vaccinations as indicated in A. B 35 patients with locally advanced TNBC were consented. Patients were excluded due to complete pathological response after neoadjuvant chemotherapy (NAC), insufficient tumor, patient withdrawal, and disease recurrence. 18 patients received personalized neoantigen DNA vaccines
Results and Discussion
A median of 21.5 somatic mutations was found per patient, eight of which led to the identification of candidate neoantigens. Most of these mutations were missense mutations, with TP53 mutations being prevalent. The inclusion of TP53-related neoantigens highlights the potential of targeting common driver mutations in TNBC. The vaccines included a median of 10 neoantigens, ranging from 4 to 20 per patient.
Forty-five out of 47 neoantigens that induced an initial response were confirmed as immunogenic. A total of 14 patients showed a response to at least one neoantigen, with 23% of the 198 total neoantigens being immunogenic. After vaccination, a marked increase in the number of spot-forming cells (SFCs) was observed in patients, indicating an expanded neoantigen-specific immune response. Flow cytometry analysis revealed both CD8 and CD4 T-cell responses to the neoantigens. The expansion of neoantigen-specific TCRs following vaccination was further confirmed, with some neoantigens showing monoclonal responses and others demonstrating oligoclonal expansion.
Clinical outcomes were assessed by comparing recurrence-free survival (RFS) in vaccinated patients to historical TNBC controls. After 36 months, vaccinated patients had an RFS of 87.5%, significantly higher than the 49% observed in the control group (P = 0.011). Vaccination was well tolerated, with one grade 3 event (hypertension) and 13 grade 2 events (injection site pain), along with mild myalgia (grade 1).
Overall, the study suggests that personalized neoantigen DNA vaccines are feasible, well-tolerated, and capable of inducing robust immune responses and improving clinical outcomes in TNBC patients. Although the trial was not randomized and comparisons to historical controls have limitations, the observed improvements in RFS strongly support further exploration of this approach.
Conclusion
In conclusion, the neoantigen DNA vaccine platform approach offers a promising, personalized immunotherapy strategy that could also be extended to other cancers with low mutation burdens, potentially improving outcomes in difficult-to-treat malignancies. Future studies combining these vaccines with immune checkpoint inhibitors may further enhance therapeutic efficacy.