New research finds that maternal stress during pregnancy and postpartum may significantly influence the gut microbiota of both mother and baby, highlighting potential long-term health risks and the urgent need for better stress management strategies.
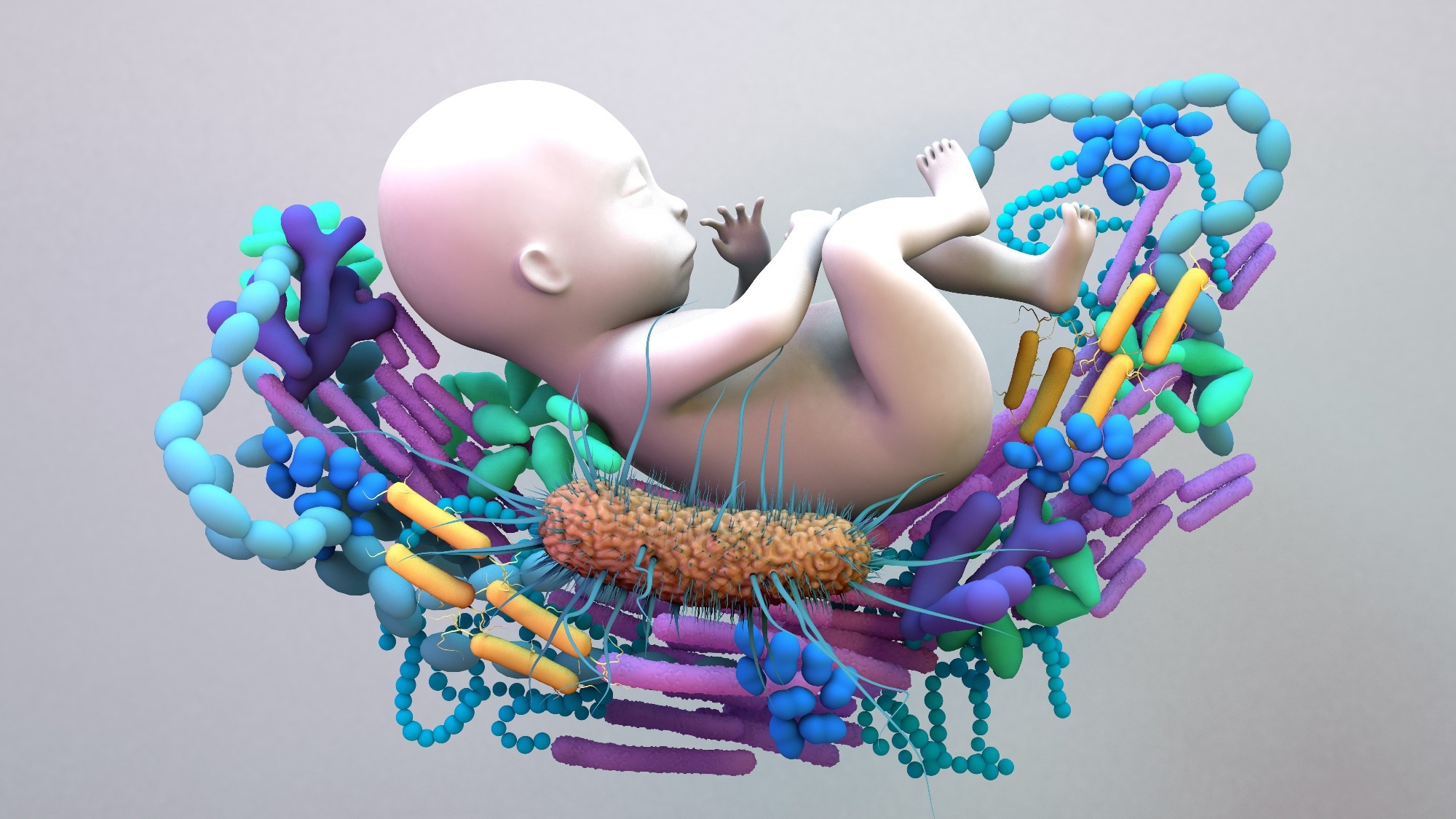 Scoping Review: The impact of perinatal maternal stress on the maternal and infant gut and human milk microbiomes: A scoping review. Image Credit: Design_Cells / Shutterstock
Scoping Review: The impact of perinatal maternal stress on the maternal and infant gut and human milk microbiomes: A scoping review. Image Credit: Design_Cells / Shutterstock
Researchers at the University College Cork, Ireland, have conducted a scoping review of existing studies describing the impact of perinatal maternal stress on the maternal and infant gut microbiota and the breastmilk microbiota. They have published this review, which systematically maps the available evidence, in the journal PLOS ONE.
Background
Pregnancy and the post-pregnancy (post-partum) period are considered a phase of significant physiological and psychological transition in women’s lives. These transitions can significantly affect women's well-being and health and influence the health and development of their newborns.
Multiple factors can trigger perinatal (the time from pregnancy until the end of the first year post-childbirth) maternal stress, including lack of social support, family and workplace responsibilities, and pregnancy- or delivery-related complications. The global prevalence of perinatal maternal stress ranges from 5% to 93%, with some studies indicating a possible increase since the coronavirus disease 2019 (COVID-19) pandemic, although the available evidence remains inconclusive.
Early-life exposure of infants to perinatal maternal stress has been found to increase the risk of various health complications, including metabolic, immunologic, and neurobehavioral disorders. The maternal microbiota plays a significant role in modulating infant health and development.
The maternal gut-microbiota-brain axis can facilitate the colonization of aberrant microorganisms in the mother’s vaginal, gut, and breastmilk microbiota, which can subsequently be transferred to infants and predispose them to more inflammatory microbiota associated with dysregulated metabolic processes and adverse health outcomes.
The current review of existing evidence aims to provide an in-depth overview of the potential impact of perinatal stress on maternal and infant health.
Review Design
The review's fundamental objective was to explore the effect of perinatal maternal stress on the maternal gut and breastmilk microbiota and the collective impact of maternal microbiota changes on the infant gut microbiota.
The authors screened various electronic databases and identified seven studies that clearly aligned with the review objective. Two of these studies investigated the impact of perinatal stress on the maternal gut microbiota, and five assessed the impact of perinatal stress on the infant gut microbiota. However, no studies were found examining the association between perinatal stress and maternal breastmilk microbiota, representing a significant gap in the research on vertical microbial transmission.
The Review Findings
Five of the seven studies analyzed by the authors showed that perinatal maternal stress significantly influences the composition of gut microbiota in mothers and infants.
Specifically, these studies showed that higher maternal stress increases the abundance of potentially pathogenic bacteria such as Erwinia, Serratia, Terrisporobacter mayombei (T. mayombie), and Bacteroides. On the other hand, lower maternal stress was found to increase the abundance of beneficial bacteria such as Lactococcus, Lactobacillus, and Akkermansia.
Only one study reported conflicting results, showing that higher maternal stress is associated with a higher abundance of beneficial bacteria.
A high level of heterogeneity in stress measurement tools and stress assessment time points was observed between the included studies, which may explain the observed variations in study findings.
The studies that used subjective scales (Perceived Stress Scale, Daily Hassles Scale, Everyday Problem Checklist) for stress measurement reported no significant impact of maternal stress on the gut microbiota composition and diversity. In contrast, studies that included additional testing, such as analysis of serum cytokines, salivary cortisol, cortisol awakening response, and hair cortisol, identified significant associations between maternal stress and gut microbiota alterations.
The major disadvantages of self-reported stress ratings include recall bias, a lack of willingness to disclose information, and a lack of representation of subconscious or physiological stress responses. As evidenced in this review, significant microbiome changes were less consistently observed in studies relying solely on self-report data, whereas studies incorporating biological markers tended to show more measurable microbiota alterations.
This suggests that different stress measurement approaches may yield different conclusions, underscoring the importance of integrating both subjective and objective stress assessments in future research.
These observations highlight the need for biomarker-based testing, such as cortisol or cytokine analysis, alongside psychological assessments to improve accuracy in stress-related microbiome research. Other significant aspects to consider include the duration, severity, and specific timing of stress exposure during the perinatal period, as these factors may differentially influence gut microbiota changes.
Two studies reported an increased abundance of pathogenic bacteria due to maternal stress. The presence of these bacteria may contribute to sustained low-grade inflammation in the gut, which has been linked to chronic inflammatory disorders such as asthma, chronic obstructive pulmonary disease (COPD), inflammatory bowel disease (IBD), and metabolic conditions.
Significance
The review identifies a potential link between perinatal maternal stress and changes in maternal and infant gut microbiota composition and diversity. However, the studies analyzed in this review indicate that maternal stress can influence bacterial colonization in different ways.
The high variability in microbiome composition across individuals and developmental stages, coupled with inconsistencies in stress measurement methodologies, poses challenges for this area of research. To improve future study designs, researchers should employ a combination of subjective psychological stress scales, biomarker-based assessments, and longitudinal sampling to track microbiome changes over time.