In this interview, industry expert Dr. Yifan Jian discusses advancements in ultrawide-field optical coherence tomography (OCT), challenges in retinal imaging, AI’s role in biophotonics, and the future of high-speed, high-resolution ophthalmic imaging.
Can you tell us about your career path and what led you to specialize in biophotonics and optical coherence tomography (OCT)?
I started my academic journey in China, where I completed my undergraduate degree in optics in Shanghai. After that, I moved to Vancouver, Canada, for my PhD, where I specialized in biophotonics. That’s when I was first introduced to OCT, its applications in eye imaging, and adaptive optics. My supervisor was one of the early researchers in OCT, so I had the opportunity to work with various OCT and imaging systems designed for the anterior and posterior eye segments.
After completing my PhD in 2014, I stayed in Vancouver for a few years before being recruited by Dr. David Huang - one of the co-inventors of OCT - at Oregon Health and Science University (OHSU). I joined the faculty to continue developing OCT and other eye imaging systems there. My career has remained rooted in academia, focusing entirely on advancing research in this field.
How have these fields evolved since you began your research?
OCT has always had a strong translational focus. Since its invention and early patenting, it has been rapidly commercialized, leading to numerous companies producing and deploying OCT systems worldwide. Today, OCT is one of the most important diagnostic tools in ophthalmology, particularly for retinal diseases. Its rise coincided with the development of new treatments for retinal conditions, such as anti-VEGF therapy. It allows doctors to determine precisely when to begin these highly effective treatments.
From a technology perspective, one of the key advancements has been the dramatic increase in OCT speed. Early systems could capture tens to hundreds of scans per second, while modern systems operate at millions of scans per second. Researchers have also worked on enhancing resolution axially and transversely using techniques such as adaptive optics.
Beyond structural imaging, new contrast mechanisms have emerged, such as OCT angiography for visualizing blood vessels and optoretinography to study how photoreceptors respond to light. Other emerging techniques include using OCT to measure oxygen saturation at the capillary level, particularly with visible light OCT.
When I moved to OHSU, my focus shifted towards expanding the field of view. Instead of zooming in to capture tiny cellular details, I worked on imaging the entire retina, providing a comprehensive view of the retinal health which is critical for clinical applications.
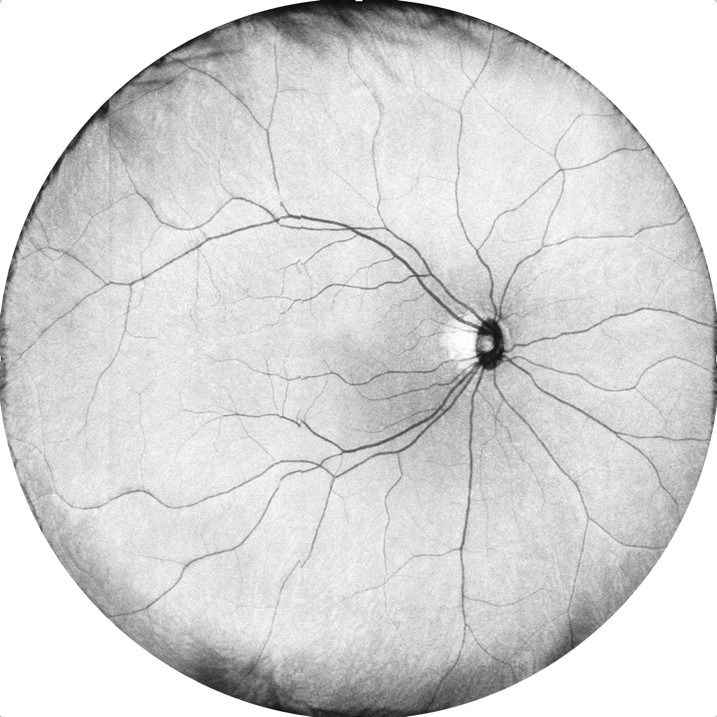
Image Credit: Dr. Jian, OHSU University
What were some key challenges in developing ultrawide-field OCT systems, and how do they advance imaging for complex retinal conditions?
Developing ultrawide-field OCT comes with multiple challenges. The first is scan time - as you increase the field of view, the system needs more time to scan the entire area and collect data. This prolongs imaging sessions, increasing the likelihood of motion artifacts and patient discomfort. The solution is higher-speed OCT systems, which we achieve using advanced laser technology.
The second challenge is the depth of imaging. The eyeball is curved, so we need a deeper imaging range as we expand the field of view. Swept-source OCT systems require high-speed digitizers and sophisticated data processing tools. We address this using GPUs to process data in real-time.
The third and biggest challenge has been optics. We needed a high-quality optical system with custom-designed lenses to effectively direct light across the entire retina. Off-the-shelf components were not designed for ultrawide-field OCT, so they did not provide the image quality we needed.
Initially, we tried adapting ophthalmic lenses used in other imaging modalities, but they were not optimized for OCT, so they lacked the necessary optical quality and performance for our ultra-wide-field imaging goals.
How did your collaboration with Avantier start, and what drew you to working with them?
When we realized that existing ophthalmic lenses were insufficient for ultrawide-field OCT, we knew we had to design and manufacture our custom optics. This required a deep dive into optical design and simulation software to develop high-performance lens systems.
As we began searching for a manufacturing partner, Avantier stood out for its ability to produce high-quality optics while remaining cost-effective. Compared to other companies, Avantier offered a reasonable and affordable approach, which was crucial for us as we ventured into custom lens design for the first time.
The results have been outstanding - our systems now provide high-quality, ultrawide-field images that are being used in clinics for conditions like diabetic retinopathy and in neonatal intensive care units to screen premature infants for retinopathy of prematurity.
This collaboration has enabled us to push the boundaries of ultrawide-field OCT, ensuring our systems achieve the highest possible performance for both research and clinical applications.

A sample picture of the eyepiece. Image Credit: Avantier
Could you discuss the significance of ultrawide-field OCT systems in retinal imaging and any recent developments from your lab in this area?
Our ultrawide-field OCT systems have significantly expanded the scope of retinal imaging. Handheld and desktop configurations allow comprehensive analysis of the anterior and posterior segments of the eye, which has important applications in conditions like diabetic retinopathy or age-related macular degeneration.
One of the biggest advancements in my lab has been developing a system that can capture a near-complete 3D reconstruction of the entire eyeball in a single scan. This technology is particularly valuable for myopia management, allowing us to track how eye shape changes.
We are also using ultrawide-field OCT in ocular oncology to precisely measure tumors inside the eye. Traditional imaging methods like MRI or ultrasound lack the resolution necessary, whereas OCT provides highly detailed structural information.
Another major focus has been increasing imaging speed. We have developed novel systems that project entire lines of light instead of scanning single spots. This allows us to acquire images in parallel, significantly speeding up the process. We are also exploring different illumination schemes to improve tissue contrast, revealing retinal layers that were previously difficult to distinguish.
What advancements do you foresee AI bringing to biophotonics?
AI has the potential to transform retinal imaging. One promising application is using AI to analyze OCT scans for signs of systemic health conditions like cardiovascular disease, Alzheimer’s, and other neurological disorders.
The retina provides a unique window into overall health - AI algorithms can extract subtle biomarkers from OCT images that are difficult for human observers to detect, which could massively enhance diagnostic capabilities.
However, for this to reach its full potential, we need widespread access to affordable OCT systems. If low-cost devices became available in places like pharmacies or optical retail stores, AI-powered OCT screening could become a routine part of healthcare, making early disease detection far more accessible.

Image Credit: Depiction Images/Shutterstock.com
Among your numerous publications, are there any particular studies or findings that have significantly impacted your field or hold personal significance to you?
One of my earliest and most impactful works was on GPU-accelerated OCT image processing. OCT generates massive amounts of data, and processing it in real time is crucial, especially for applications like neonatal imaging, where infants won’t stay still for long. Traditional CPUs weren’t fast enough, so we developed a system that uses GPUs - specifically NVIDIA video cards - to dramatically speed up the process.
This real-time image processing capability changed how we use OCT. It allows clinicians to see cross-sectional and 3D retina views instantly while scanning, providing immediate feedback for diagnosis. The software we developed over a decade ago is still widely used in research labs worldwide today.
My research on adaptive optics for high-resolution imaging was another significant contribution. We developed a system that does not rely on wavefront sensors but instead iteratively optimizes image quality. This technique has been successfully applied to small-animal imaging.
My work on retinopathy of prematurity has been particularly meaningful more recently. Using ultrawide-field handheld OCT, we have redefined the disease’s diagnostic criteria, identifying new biomarkers that were previously undetectable with conventional imaging - this could improve early diagnosis and treatment.
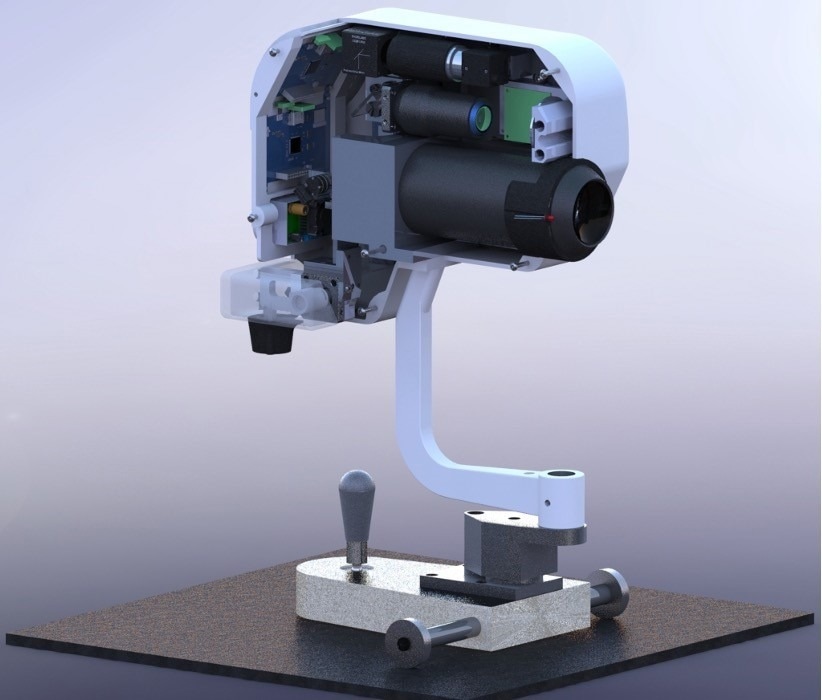
Image Credit: Dr. Jian, OHSU University
What’s your vision for the future of OCT and other imaging technologies in the next 5–10 years?
I see speed as the defining factor in the future of OCT. Current commercial systems are still relatively slow compared to research-grade devices. Higher-speed OCT will allow for larger field-of-view imaging and functional assessments such as optoretinography, which can evaluate photoreceptor function in real time.
In research, we will continue pushing for higher resolution and better contrast mechanisms, such as oxygen saturation mapping. Thoughtful optical design will be critical to push the limits of what OCT can reveal.
What advice would you give students or early-career researchers interested in biomedical imaging?
I encourage young researchers to focus on projects with strong translational potential. In a clinical setting, you see real-world challenges in diagnosis and treatment - our role as researchers is to develop solutions that can make a real impact.
Working on technologies that can be applied within a 5–10-year timeframe is incredibly rewarding. Whether in academia or industry, prioritizing research that can improve patient outcomes is the best way to contribute meaningfully to the field.
About Dr. Yifan Jian 
Dr. Yifan Jian is an Associate Professor at Casey Eye Institute specializing in optical imaging. He earned his Ph.D. from Simon Fraser University in 2014 and later joined Oregon Health and Science University (OHSU) to advance OCT technology for ophthalmic imaging, including real-time processing and adaptive optics innovations. Currently, his main research focus is advancing ultrawide-field OCT systems.