Reviewed by Maria OsipovaJun 12 2023
The failure rate of novel cancer medicines remains exceptionally high, with around 95% of compounds tested in clinical trials never becoming a medicine, despite all seeming promising in the discovery lab and during preclinical work.
The underlying problem is that early testing may be good at demonstrating that a compound can destroy cancer cells in a preclinical model system. These models do not identify those likely to be equally successful when administered to humans.
The questions posed are:
- Should we continue to drive anti-cancer drug candidates into the clinic with the knowledge that 95% of them will only cause side effects to patients enrolled in early phases of clinical trials?
- Should we continue such financial expenditure for so little clinical value?
- Should we continue to choose drug candidates with the same preclinical trial systems?
Oncodesign Services does not wish to continue in this manner. The company constantly pushes alternative models and technological advances into the preclinical drug development process, intending to reverse this virtuous trend, limiting failures in late-stage studies, and minimizing the potential for harm in clinical trials.
The unique preclinical cancer model does not exist
The use of panels of models is still required, with each model having its limitations and each patient having unique cancer features.
Numerous research papers utilize animal models, emphasizing that these models continue to play a fundamental part in translational medicine, even in a historical moment when there is a growing need to discover alternative methodologies.
For decades, in vivo models have been heavily utilized. These models involve tumors being engrafted in rats or mice. The rodents are required to be immunodeficient to engraft human tumors in them.
The immune system plays a significant part in cancer, and many drugs targeting the human immune system are currently available for cancer treatment. Due to the xenografted rodents having weak immune systems, an essential component of the model is missing.
To counter this, re-introducing human immune cells into mice with human tumors may improve the representation of clinical reality and make them slightly more predictive of what might occur in the clinic.
Combining these “immune-humanized” mice with patient-derived xenograft (PDX) tumors taken directly from the patient, instead of historical in vitro cultured cancer cells, should noticeably improve the identifications of patients who would be more likely to respond to a novel treatment.1
While this retains the tumor’s histology and genomic situation, it is still insufficient since several tumor micro-environment components are not included.
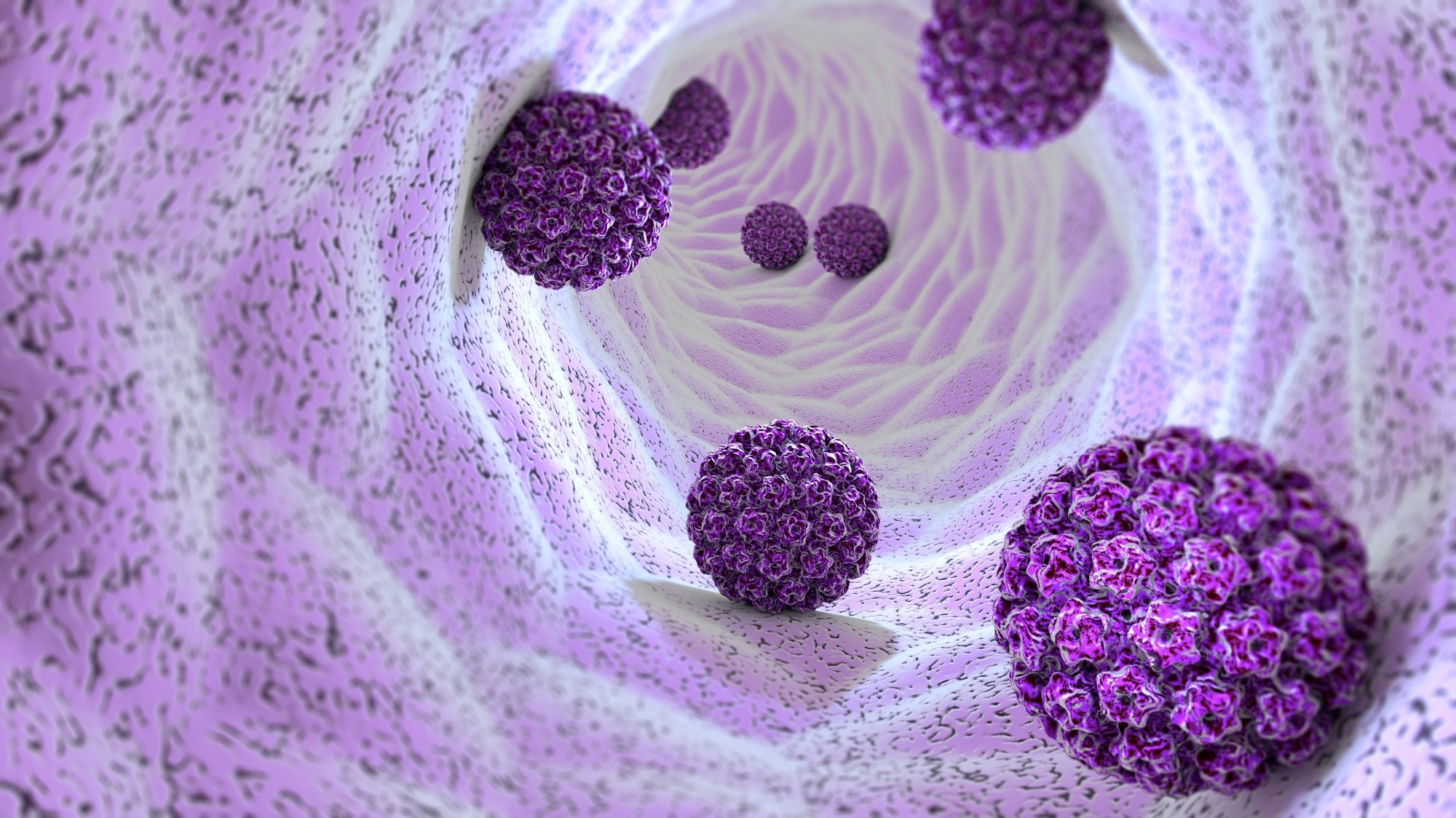
Image Credits: Naeblys / Shutterstock
Can we continue to humanize animals?
Giving the animals human immune cells and an engrafted human tumor results in a more realistic but complex model.
A “hot” immune-infiltrated patient tumor continues to be “hot” when engrafted in immune-humanized mice. In reverse, a “cold” immune-infiltrated patient tumor continues to be “cold” when engrafted in immune-humanized mice.
These results show that the human tumor cells can educate and drive the human immune cells in a murine host.
It has also been shown that aggressive chemotherapies or the tumor alters the gut microbiota (with bacteria as the most populous community) of patients or tumor-bearing mice.
These alterations affect the tumors’ response to cancer immune therapies, such as anti-PD1. This tumor sensitivity to immune checkpoint inhibitors should be reinstated via re-engrafting human-beneficial bacteria in mice.
The liver of mice may also be humanized to improve predictions of drug metabolism and possible drug toxicities and to put all these human components into one animal.
Despite this being more ‘human’, another problem persists: the process of humanization of the cancer-associated fibroblasts (CAF), a component that represents between 10% to 80% of the tumor stromal compartment, is still unknown.
This means that when patient-derived tumors are engrafted in mice, the human fibroblasts are rejected and replaced by murine ones. The gap between rodents and human still needs to be closed.
The development of novel drug candidates without consideration of the cancer metastasis process
The majority of cancer deaths are in patients who will have developed metastases. Preventing metastasis would make cancer significantly simpler to treat and even cure. However, few models are effective at the identification of the metastatic potential of a tumor.
The key to metastasis appears to lie in the interaction of the tumor cells with its microenvironment, such as the fibroblast, the immune cells, the microbiota, the host natural organ cells, etc.
In syngeneic models, where mice have a complete microenvironment with the same tumor cell origin but the tumor is not human, it is considerably more likely to metastasize than the xenogeneic models, where the origin of the tumor cells and the microenvironment are different.
At Oncodesign Services, it is also known that rat tumor models are superior as predictive pharmacological models than that of mouse models. However, many drug manufacturers remain reluctant, incriminating the size of animals that should affect the number of compounds and the budget required for preclinical development.
Over the next decade, the preclinical oncology models will likely need to be changed, or at least need the paradigm to be reconsidered, to increase the chances of clinical success and advantages for the patients.
Cancer is generally recognized as an ecological and evolutionary process with intricate interactions between tumor cells and their environment sharing numerous similarities with organismal evolution.
This is usually scrutinized as a pathological process that is characterized by chromosomal aberrations and clonal expansion subject to stochastic Darwinian selection within adaptive cellular ecosystems.
Developing tumor models that better reflect human biology continues to be a work in progress
This is a critical problem to solve if we are to improve predicting the likelihood of a compound becoming an effective anticancer drug and decrease the vast attrition rate of molecules in the clinic.
Oncodesign Services has been developing models since 1995, including chemo-induced syngeneic to xenogeneic, such as genetically modified, immune-humanized, and PDX in vivo models. The company’s extensive knowledge covers an expansive in vivo and in vitro pharmacological scope.
Oncodesign Services recently developed in vitro human tumor organoids, referred to as “tumor-on-chip”, and these are now becoming robust systems for the evaluation of anti-cancer drug efficacy.
In a recent publication, Wang et al. demonstrated the immense value of patient lung cancer organoids as an effective in vitro system for predicting and personalizing cancer treatment for patients with lung cancer.2
These models are increasingly robust and complex, but no one is producing realistic predictions of the clinical benefits of a new drug candidate using these alone.
Oncodesign Services believes that a combination of models is essential to enabling the selection of better drug candidates and an improved image of clinical predictivity, as proven by Hoare et al.3
Hoare et al. showed the complementarity of three varying types of preclinical models of pancreatic adenocarcinoma (ex vivo organoids, in vivo PDX, and in vitro primary tumor cells from the same patients) for the first time.
This is why Oncodesign Services has invested 30 years in developing a holistic and comprehensive preclinical platform with a substantial panel of technologies around its cancer models, such as genomics, proteomics, and pharmaco-imaging.
The company hopes that applying data-driven “artificial intelligence” technologies will aid improved characterized human-like models and analysis of these complicated combinations of models to evade misleading conclusions and the subsequent overlooking of clinically relevant features.
Oncodesign Services places much importance on patients eagerly awaiting the solution to cure their cancer.
Acknowledgments
Produced from materials originally authored by Olivier Duchamp at Oncodesign Services.
References:
- Julien et al., Clin Cancer Res, 2012
- Cell report, 2023
- Cancer, 2021
About Oncodesign Services
Oncodesign Services is a Contract research organization (CRO) specializing in drug discovery and preclinical services. From target identification to IND filing, the company contributes to the development of innovative therapies in oncology, inflammation and infectious diseases, with high medical needs.
Through integrated capabilities in medicinal chemistry, DMPK, pharmaco-imaging, bioanalysis, in vivo/In vitro pharmacology, Oncodesign Services support the R&D programs of customers with a global footprint.
Based in Dijon, France, in the heart of the university and hospital cluster and within the Paris-Saclay cluster, Oncodesign Services has 230 employees in France, Canada and the United States.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.