Children spend much time away from home, whether at clubs, nursery, or school, and it is crucial to ensure their safety when away from home. Children with asthma, therefore, require responsible adults around them to understand what to do in an asthma emergency.
How common is asthma?
Asthma is a widespread respiratory condition affecting approximately 5.4 million people in the UK, and 1.1 million are children.1,2 Asthma is the most widespread long-term condition among young people, and the UK has among the highest European mortality rates. Emergency admissions and deaths linked to asthma are considered largely avoidable, with these numbers being associated with deprivation.2 There was reportedly a small decline in deaths among children and young people linked to asthma between 2008 and 2018. Although the figures are low, they are still excessively high for an illness that should be manageable, making the deaths preventable.3
The trend sadly appears to rise among 15 to 24-year-olds.3 A report in 2019 showed that among 19 countries, young people are more likely to die from asthma in the UK compared to those in other wealthy countries.4 This is unacceptable and requires improvement.
What is asthma?
The British Thoracic Society and Scottish Intercollegiate Guidelines Network guidelines define asthma as presenting at least two of the following symptoms:
- Wheezing
- Breathlessness
- Chest tightness
- Coughing
Asthma exhibits different symptoms, which could vary over weeks or months. The fundamental problem lies in the airways, which can be hyperresponsive or inflamed.
What symptoms do asthma sufferers typically suffer from?
The most widespread symptoms of asthma include:
- Coughing
- Wheezing
- Shortness of breath
- Limited exercise capacity,
- Duration of symptoms
- Triggers
Hopefully, no one suffers from all of the above. Symptoms are variable and can come and go over time. It is relatively common for a person to know what triggers their symptoms.
How does asthma impact the lungs?
Asthma leads to inflammation of the mucous membrane, which can result in swelling of the airspace, increased mucus production, twitching airways, and bronchospasms.
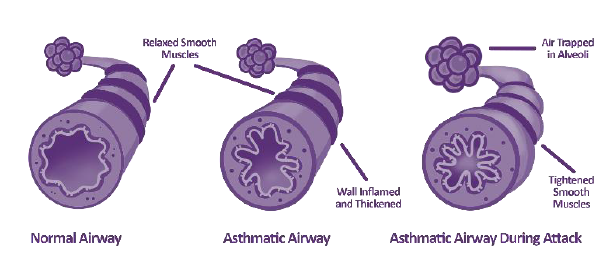
Image Credit: Bedfont® Scientific Ltd
Watch the webinar: Children with Asthma
How is asthma measured?
Asthma can be measured or monitored in several different ways. The first method is via a peak expiratory flow meter. This is a simple test involving a device with a scale. First, one should ensure the slide on the scale is on 0. Then, a deep breath should be taken, followed by a short, sharp blow into the meter.

Image Credit: Bedfont® Scientific Ltd
Another method for measuring asthma is spirometry, which involves a more sophisticated look at how air moves in and out of the chest. It assesses how much air moves out of the chest, how quickly it can be done, and the pattern the air takes as it exits the chest. This test should be undertaken in a clinic.

Image Credit: Bedfont® Scientific Ltd
There is also a fractional exhaled nitric oxide (FeNO) test. Humans generally produce small amounts of NO in their breath, but more NO is produced when a patient has chest inflammation, such as the type often seen in patients with asthma.
A FeNO test undertaken by NObreath® is appropriate for both adults and children. It requires patients to take a deep breath in and blow into the device at a steady pace
Asthma is a serious, long-term condition, and insufficiently controlled asthma may present physical symptoms. When present in children, these can include:
- Shortness of breath
- Chest tightness
- Wheezing
These symptoms can lead to further complications in children. If they feel sick, they are less likely to participate in physical activity, which can lead them to become deconditioned and at a higher risk of obesity, which can, in turn, worsen asthma. Inadequately controlled asthma may interfere with sleep, impacting concentration, emotions, and behavior.
Poorly controlled asthma can also have psychological effects on children. Children usually like to be like other children, and having asthma may make them feel different. They may be embarrassed by their inhaler, meaning they do not use it when they should.
They might have experienced an asthma attack in the past, and it might make them frightened to do things that may trigger another attack, limiting them in what they feel they can do.
Inadequately controlled asthma can also affect education outcomes, as children with asthma may be absent from school for medical appointments or asthma attacks. They might also have reduced concentration due to disturbed sleep or feeling unwell.
How is asthma treated?
Approximately 119 different inhalers are available, meaning many treatments and options exist for people with asthma. Bedfont Scientific hopes that anyone with asthma has:
- No symptoms during the day
- No symptoms during the night
- No limitations to activity
- No need for a rescue inhaler
- No side effects stemming from treatment
- Normal lung function
When treating asthma, it is crucial to treat the underlying inflammation. If treatment is done correctly, the swelling reduces, the airways open back up, and the patient finds breathing easier.
Not all treatments are instant, however. If a brown-colored preventer inhaler is used, for example, it should be used for a few days. This enables the medication to reduce the inflammation slowly, and once settled, it is likely to be needed long-term.
There are two categories of inhalers:
Treatment:
- Treats underlying inflammation
- Reduces swelling
- No instant effect
- For long term management
Rescue:
- Treats twitchy airways
- Fast symptom relief,
- Should only be needed occasionally
- Lasts a maximum of four hours
Image Credit: Bedfont® Scientific Ltd
Using a blue rescue inhaler more than three times a week indicates inadequate treatment and a need for reassessment. It is vital to know the difference between the treatment inhaler—typically orange and brown in color—and the rescue inhaler, which is always blue.
Maintenance and reliever therapy is a combination inhaler and may also be used. The inhaler consists of treatment and rescue medications and is used regularly twice daily if symptoms occur. Further doses of this inhaler should only be required on occasion.
It is vital to use the inhaler correctly. Unfortunately, many people do not know how to use inhalers correctly, partially due to a lack of advice from their healthcare provider. This shows that education is crucial for patients to take their medication properly.
Types of inhalers:
- Pressurized metered dose inhaler
- Spacer devices
- Breath-actuated meter dose inhaler
- Dry powder inhaler
It is vital to be aware of the different types of inhalers and the right way to use them. If one has a metered-dose inhaler, the breathing technique should be slow and gentle.
If one has a dry powder inhaler, breathing in fast and hard is necessary. If one uses the fast and hard technique with a metered dose inhaler, the medication will hit the throat rather than enter the lungs. Likewise, dry powder inhalers will not move the powder into one’s lungs if one does not breathe fast and hard.
Spacers are available, typically for children. They are chambers for metered dose inhalers to reduce the medication’s speed and hold it for a few seconds, providing more time for the user to inhale. Many different sizes of spacers are available, varying according to the age and capability of the users.
What if my asthma is not that good?
Even if all of the previous steps are in place and one’s treatment is correct, asthma may still flare up. If this occurs, steps can be taken to tackle it.
- Use treatment inhalers regularly
- Know how to use an inhaler optimally
- Be aware of triggers,
- Book a review with the asthma nurse,
- If using a blue rescue inhaler exceeds three times a week, book an appointment
- In case of shortness of breath not improved by using an inhaler, make an urgent GP appointment for the same day
Watch the webinar: Children with Asthma
What should be done during an asthma attack?
Knowing what to do during an asthma attack may be the difference between life and death. The graphic from Asthma + Lung UK below demonstrates the steps to take during an attack.
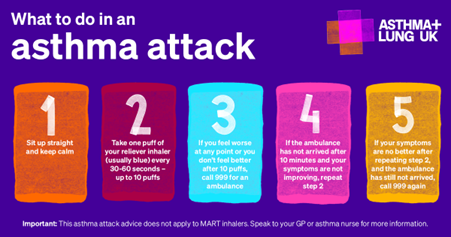
Image Credit: Asthma + Lung UK
To ensure adequate care, everyone should have a personalized asthma action plan. Different formats are available. Below is an example from Asthma + Lung UK:
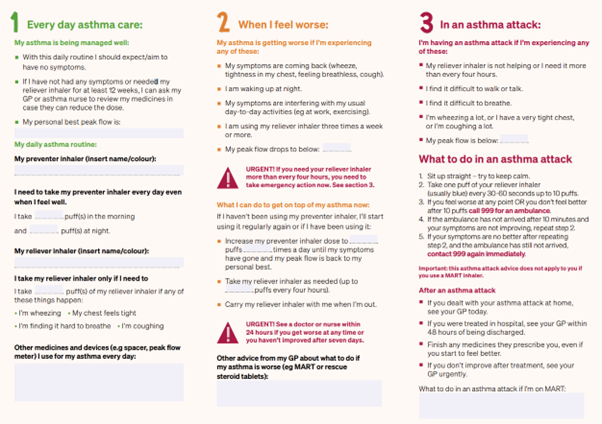
Image Credit: Asthma + Lung UK
The green region is when asthma is under control. This is how it feels when asthma symptoms are checked, and this medication should be taken to maintain good asthma control.
Amber represents when things are beginning to worsen. A key question is, “How is it possible to recognize when symptoms are beginning to deteriorate?” The guide provides steps to improve symptoms and switch back to green.
Red indicates an asthma emergency and what should be done in this situation.
It is vital to recognize when one is in the red zone and what to do if this happens. It is also good to realize that when one is in the amber region, one may be able to get back into the green zone.
Seasonal Variations
There are seasonal variations as to when hospitals see peaks in asthma admissions. These may occur during:
- Fall: Back to school
- Winter: Winter colds
- Spring: Pollen
The UK pollen calendar demonstrates peaks in spring and throughout the year.

Image Credit: Worcester University
What can trigger asthma?
Various triggers for asthma exist, however, the most widespread include:
- Anger
- Bugs in the home
- Cold air
- Dust
- Exercise
- Fumes from chemicals
- Fungus spores
- Pets
- Pollution
- Smoke
- Stress
- Strong odors
Some lesser-known triggers include:
- Alcohol
- Damp and mold
- Drugs
- Hormones
- Infection
- Sex
- Some foods
- Temperature changes
- Thunderstorms
How can the effects of triggers be managed?
Sometimes, little can be done to avoid triggers. Where possible, however, they should be eliminated or avoided. Other conditions that trigger asthma should be treated, and ensuring asthma is well-managed is crucial.
Triggers can be predicted. If hay fever is a trigger, treatment should start early. It is essential always to keep rescue medication within easy access.
Parents and carers should understand asthma to understand how the medication works and why it is crucial. They should have an asthma action plan, know how to maintain control, and what to do in case of an emergency. They should also know what to do if an inhaler has been forgotten.
Given that asthma is still an ongoing serious respiratory condition that kills children each year, this webinar has helped people understand the following:
- Asthma and the treatment
- The goals of the treatment
- How and when to use inhalers
- What to do in an emergency
- Why asthma worsens
Click here to watch the full webinar and gain in-depth insights.
Watch the webinar: Children with Asthma
References and further reading
- Asthma + Lung UK (2021). What Is Asthma? [online] www.asthmaandlung.org.uk. Available at: https://www.asthmaandlung.org.uk/conditions/asthma/what-asthma.
- Royal College of Paediatrics and Child Health (2020). Asthma – RCPCH – State of Child Health. [online] stateofchildhealth.rcpch.ac.uk. Available at: https://stateofchildhealth.rcpch.ac.uk/evidence/long-term-conditions/asthma/.
- Chen, W.-Y., et al. (2021). Decreasing ten-year (2008–2018) trends of the prevalence of childhood asthma and air pollution in Southern Taiwan. World Allergy Organization Journal, [online] 14(5), p.100538. https://doi.org/10.1016/j.waojou.2021.100538.
- Asthma: Young people in the UK ‘more likely to die’. (2019). BBC News. [online] 20 Feb. Available at: https://www.bbc.co.uk/news/health-47292157.
About Bedfont® Scientific Ltd
Bedfont® Scientific has specialised in the design and manufacture of exhaled breath and gas monitoring instruments since 1976.
For medical gas monitoring, their Medi-Gas Check medical pipeline testing range verifies not only the quantity but also quality of gas administered to patients.
Bedfont's breath analysers include carbon monoxide (CO) monitors such as the Smokerlyzer®, used for smoking cessation, and the ToxCO®, used by emergency services, to diagnose CO poisoning.
The NObreath® FeNO monitor provides accurate analysis of airway inflammation for the control of asthma, and the Gastrolyzer® range aids in the detection of gastrointestinal disorders and food intolerances. Quick and non-invasive, breath analysis is the new blood test.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.