Screening means looking for the cancer or ailment before a person has any symptoms. This can help find cancer at an early stage. If any abnormality is detected early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread and may become more difficult to treat increasing health care costs and shortening lifespan.
Breast cancer screening
Breast screening is a method of detecting breast cancer at a very early stage. A mammogram is the first step in screening. It is an x-ray of each breast taken while carefully compressing the breast. The mammogram can detect small changes in breast tissue that may need further investigations to check for cancer.
When to screen for breast cancer
In the United Kingdom, most women receive their first invitation to attend for a mammogram at the local breast screening unit sometime between their 50th and 53rd birthdays. The screening invitations are sent out every three years till a woman is 70.
Women under 50 are not currently offered routine screening. Studies have shown that routine screening in the 40 to 50 age group is less effective. After menopause the glandular part of the breast reduces and is replaced by fatty tissues. This makes the breast less dense and makes interpretation with mammograms easier.
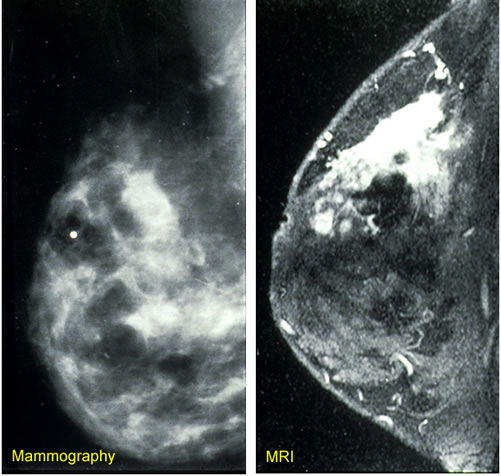
Example breast imaging technology
Digital mammography however is better for screening younger women and women with denser breasts, and is equally effective as film mammography in older women. Women over 70 are not sent routine invitations, but may request three-yearly screening visits.
At the screening unit
Before mammography, a detailed history of breast diseases in the woman or in her family is obtained. All women are taught to be breast aware between two screening visits. This means all women have different consistencies and “feel” of their breasts. They should be aware of how their normal breast feels to be able to detect an abnormality at the earliest. All women are taught to regularly perform Breast Self-Exam.
Mammogram
The mammogram is a low dose x-ray. Each breast is placed in turn on the x-ray machine and gently but firmly compressed with a clear plate. This lasts for a few seconds and is harmless. This pressure helps to keep the breast still and get a clearer picture using lowest amount of radiation. It may be slightly uncomfortable or painful much like while measuring blood pressure and is less painful than a blood test. The mammograms are examined and the results sent to the woman and her practitioner.
Further investigations
If the mammograms show positive findings, the woman is asked to return for further investigations. These may include:
- a clinical examination
- mammograms at different angles or with magnification
- examination using breast ultrasound
- an MRI image
- fine needle aspiration or core biopsy
- open or excisional biopsy
Treatment options
Once cancer is confirmed the woman is referred to a consultant surgeon for a discussion of the options available to her. This is essential before making any decisions on treatment.
Treatment may involve surgery, likely to be followed by radiotherapy, chemotherapy or hormone therapy or a combination of these. The exact course of treatment will depend on the type of cancer found and the woman's personal preferences.
Those at high risk
All women identified as being at higher risk include those with a family history of breast cancer (in their mother, daughter or sister). They need to be assessed for their exact risk and their risk management options need to be discussed with them. These women may be screened with digital X-ray mammography and magnetic resonance imaging. They may also need genetic screening looking for genetic mutations such as those for BRCA1 and BRCA 2.
Further Reading
Last Updated: Jun 22, 2023