Adoptive T cell therapy is a type of immunotherapy that has the ability to target cancer cells through inherent mechanisms of the immune system. The method works by infusing tumor-specific cytotoxic T cells into patients that will recognize, target, and attack tumor cells.
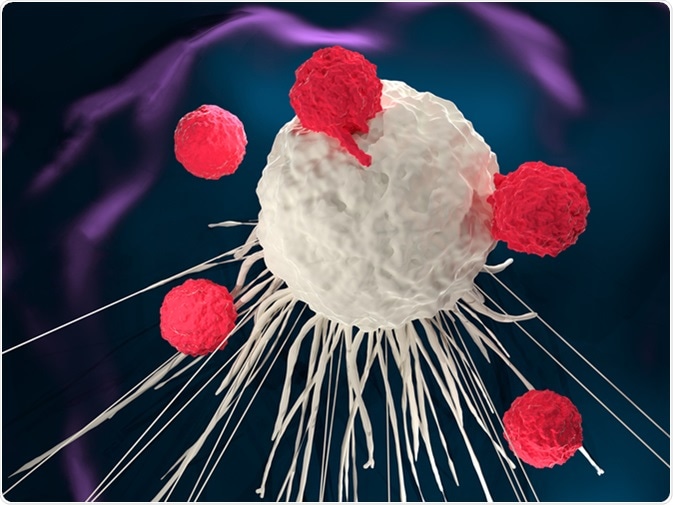
Image Credit: Meletios Verras / Shutterstock
Type of therapies
Adoptive T cell therapy methodologies include:
- Producing cultures of tumor-infiltrating lymphocytes.
- Expanding one particular T cell or clone.
- Utilizing engineered T cells that have been designed to target and attack tumors.
Adoptive T cell therapies range from the broad T cell recognition capacities of tumor infiltrating lymphocytes to a specific antigen response that is achieved through the use of engineered chimeric antigen receptor (CAR) T cells. The active immunization tha tis produced through developing cancer vaccines is also being trialed through the evaluation of adoptive T cell therapy.
Adoptive Cell Therapy: Turning Immune Cells into Cancer Fighters
Adoptive T cell therapy and tumor infiltrating lymphocytes (TIL)
The adoptive T cell therapy methodology that has the most extensive clinical history and demonstrated clinical response rates is the adoptive transfer of autologous tumor-infiltrating lymphocytes (TIL). TILs are extracted from tumors and cultured with interleukins, which are a type of cytokine messenger molecule, to form therapeutic TILs.
The TILs are then infused back into the patient, where they re-infiltrate the tumor and cause tumor regression through the lysis of tumor cells. The earliest studies of infused TILs with interleukin (IL)‐2 were found to be 50-100 times more effective in destroying tumor cells than lymphokine‐activated killer (LAK) cells.
The adoptive T cell treatment requires patient-specificity, as TILs cultured from human tumors are only able to lyse autologous cells from the same individual, but not allogeneic cells. Utilizing TILs for adoptive T cell therapy has the advantage of providing broad T-cell recognition for many tumor antigen types, rather than the single specificity capacity of other therapeutic approaches.
Current studies are attempting to minimize the time taken to culture TILs, improve the effector characteristics of T cells and identify biomarkers that allow for the selection of the most suitable patients who will respond well to this type of immunotherapy.
CAR T cell therapy
CARs are engineered to redirect T cells to recognize and attack cancer cell targets. This type of therapy involves the collection of T cells from the blood of the patient or donor. The T cells are then genetically engineered to produce the specific surface receptors needed to allow the T cell to recognize and bind to specific cancer cell antigens. Viruses are often used as vectors for delivering the genes that are required to engineer the CAR T cells.
Once engineered, the CAR T cells are then cultured within the laboratory before they can be infused into the patient. The further multiplication of CAR T cells can occur within the patient's body to ultimately create an effective immunological treatment for hematologic malignancies.
Current studies are adapting this methodology to improve success rates in solid tumors by combining CAR T cells with other effector molecules.
Adoptive T cell therapy and cancer vaccines
Another method of adoptive T cell therapy is to remove T cells from the blood of patients who have received a cancer vaccine. The advantage of this technique is that by supplying active immunization in rare tumor antigen-specific T cells, an effective therapy can be produced by expanding the number of primed T cells in the laboratory prior to infusion. One approach is to utilize tumor specific CD4+ Th1 cells for adoptive T cell therapy.
Th cells have wide functionality including the activation of antigen-specific effector cells and immune system cells, such as microphages, for antigen presentation.
By priming with antigens, Th cells are able to directly activate tumor antigen-specific cytotoxic T cells. The activation of these cells helps to broaden immunity to other antigens within the tumor. This extended immuno allows the resulting epitope to spread, which has been shown to ultimately increase the survival benefit in post-immunotherapy trials for melanoma and breast cancer.
References
- Perica, K. et al. 2015. Adoptive T Cell Immunotherapy for Cancer, Rambam Maimonides Medical Journal, 6, e0004. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4327320/
- Wu, R. et al. 2012. Adoptive T-cell Therapy Using Autologous Tumor-infiltrating Lymphocytes for Metastatic Melanoma: Current Status and Future Outlook, Cancer Journal, 18, pp. 160-175. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3315690/#R63
- D’Aloia, M.M. et al. 2018. CAR-T cells: the long and winding road to solid tumors, Cell Death and Disease, 9:282. https://www.nature.com/articles/s41419-018-0278-6
- Bonifant, C.L. et al. 2016. Toxicity and management in CAR T-cell therapy, Molecular Therapy Oncolytics, 3: 16011. https://www.sciencedirect.com/science/article/pii/S2372770516300353
- UW Medicine: Cancer Vaccine Institute. https://depts.washington.edu/tumorvac/research/t-cell-therapy
Further Reading
Last Updated: Mar 18, 2021