New research shows that GD2 CAR-T cell therapy offers a potential cure for neuroblastoma, with some patients achieving long-term remission for over a decade—marking a major milestone in solid tumor treatment.
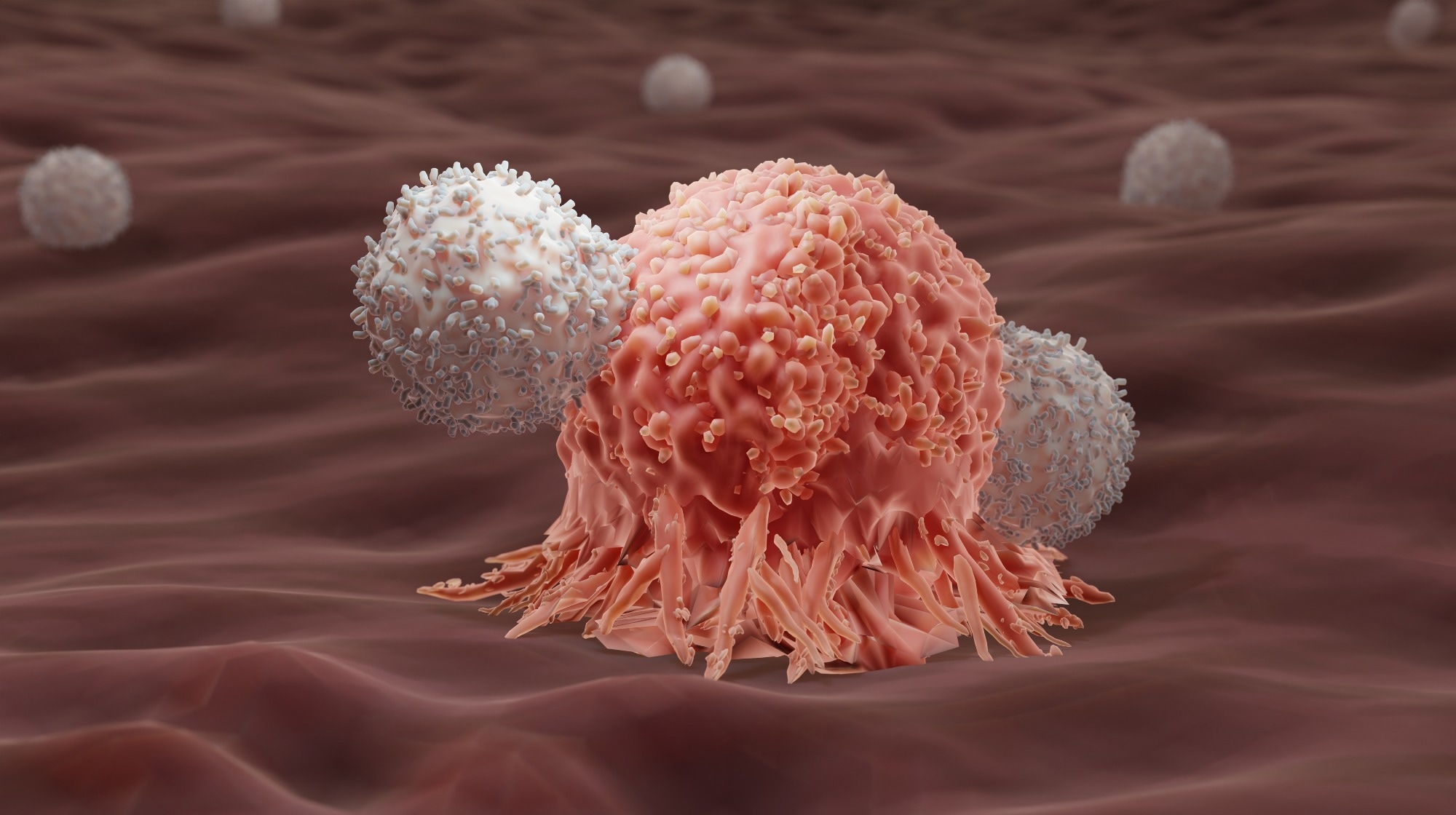 Study: Long-term outcomes of GD2-directed CAR-T cell therapy in patients with neuroblastoma. Image Credit: ART-ur / Shutterstock.com
Study: Long-term outcomes of GD2-directed CAR-T cell therapy in patients with neuroblastoma. Image Credit: ART-ur / Shutterstock.com
In a recent study published in Nature Medicine, researchers report the successful treatment of a neuroblastoma patient with chimeric antigen receptor (CAR) T-cell therapy.
What is CAR-T-cell therapy?
In CAR-T-cell therapy, T-cells are isolated from the patient’s blood and genetically engineered to express CARs on their surface. When administered to the patient, CAR-T-cells recognize and facilitate the clearance of cancer cells by binding to specific proteins on their surface.
To date, six CAR-T cell therapies have been approved by the United States Food and Drug Administration (FDA) to treat lymphoma, leukemia, and multiple myeloma. These FDA-approved therapies target CD19 or B-cell maturation antigen (BMCA) B-cells, both of which are markers that are often limited to B-cells, thereby reducing the potential toxicity of this therapy to other tissues.
Although CAR-T-cell therapy has been widely successful in treating hematological cancers, this treatment approach is limited in its ability to combat solid tumors. Some of these limitations include antigen selection, tolerability, and safety concerns, which necessitate additional studies to improve the design of CAR-T-cells to achieve enhanced therapeutic efficacy and safety.
CAR-T-cell therapy and neuroblastoma
Neuroblastoma is a rare solid tumor that develops in immature nerve cells. This type of cancer primarily affects children five years of age and younger and is associated with high relapse rates.
Between 2004 and 2009, the researchers of the current study conducted a phase I clinical trial. During this trial, activated T-cells were engineered to target disialoganglioside 2 (GD2), a protein often overexpressed in neuroblastoma cells. This therapy involved both activated T-cells (ATCs) and Epstein-Barr virus (EBV)- specific T-cells (VSTs), which were trained to recognize and attack tumor cells.
After the infusion, the CAR transgene remained detectable in the patient’s blood for over 192 weeks. To expand upon these results, the researchers of the current study provide long-term follow-up data 13-18 years after the initial infusion on the clinical outcomes of treated patients and the biological effects of this treatment approach.
Trial findings
The trial enrolled a total of 19 children, 11 of whom had active relapsed neuroblastoma. Among eight patients with no evidence of active disease, five had a history of relapsed disease, and three were infused with the GD2 CAR-T cell therapy after completing therapy for high-risk disease.
Among eleven patients with active disease at the time of infusion, three had complete responses, and one had a partial response. One of the three patients with complete responses subsequently experienced disease relapse. However, the remaining two patients had sustained responses. One experienced beneficial effects for eight years until being lost to follow-up, while the other continued to report positive outcomes for more than 18 years.
Among eight patients with no evidence of active disease at the time of infusion, five remained disease-free for up to 15 years after infusion. At the 15-year follow-up visit, event-free survival was 32%, whereas overall survival was 37%.
Of 19 enrolled patients, 12 died between two months and seven years after infusion due to relapsed neuroblastoma.
The patient who achieved more than 18 years of complete remission after the infusion never required any other cancer treatment. In fact, this female patient has completed two successful pregnancies with healthy infants. Nevertheless, this patient experienced some health adversities, including sensorineural hearing loss, which was attributed to previous chemotherapy.
Low levels of the GD2 CAR transgene were detected in patient blood samples, which likely represent CAR-T cells that persisted for at least five years. The presence of long-persisting CAR-T cells was significantly higher among long-term survivors.
Conclusions
The current study provides evidence on the long-term survival of children with neuroblastoma who received GD2 CAR-T cell therapy. Notably, the researchers reported a patient's complete remission of cancer for more than 18 years, which is likely the longest reported remission in a patient with a solid tumor treated with CAR-T cell therapy.
The trial used first-generation CAR-T cells that lack the co-stimulatory molecules currently included in advanced CAR-T cells. Thus, the intermittent low levels of CAR transgene detected during the trial follow-up period may be due to the lack of these co-stimulatory molecules. Nevertheless, the significantly greater persistence of transgenes observed in long-term survivors highlights the significance of CAR-T cells in long-term disease control.
The study findings suggest that GD2 CAR-T cell therapy is safe and has the potential to provide more than 18 years of complete remission in children with relapsed neuroblastoma without causing long-term complications.
Journal reference:
- Che-Hsing, L., Sharma, S., Heczey, A. A., et al. (2025). Long-term outcomes of GD2-directed CAR-T cell therapy in patients with neuroblastoma. Nature Medicine. doi:10.1038/s41591-025-03513-0