In critical care units, electroencephalography (EEG) can be used to observe the hidden consciousness of a patient who has suffered a brain injury and become unconscious and unresponsive.
This observation can be used to predict a patient’s possibility to regain consciousness.
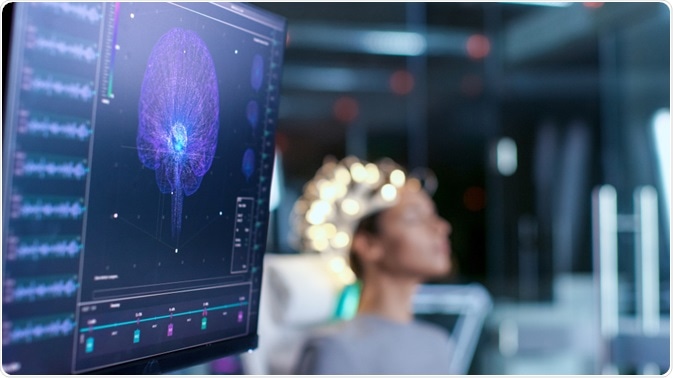
Image Credit: Gorodenkoff/Shutterstock.com
Why is EEG-based detection of consciousness is important?
The most challenging problem for a doctor in a critical care unit is to decide whether to continue life-supporting treatments for a patient who recently has suffered a critical brain injury.
For patients who have very little chance of recovery, the decision to withdraw the life-support is usually made within the first few weeks after the injury. Various techniques, such as neuroimaging, neurological and electrophysiological estimations, and routine laboratory assessments, are used to predict the possibility of recovery. However, the use of these tests alone is not completely accurate.
Patients who remain unresponsive for a prolonged period do not respond to spoken commands. However, some recent studies have shown that about 14% of these patients can have brain activation in response to spoken commands, which can be detected using EEG or magnetic resonance imaging (MRI). For an unresponsive patient with hidden cognitive abilities, a delayed recovery is possible.
Studies have found that patients remain unresponsive to commands because of the cognitive-motor dissociation. This means the brain may be able to process motor commands but not act on them.
Such dissociation can be present for months to years after a brain injury. Thus, an accurate prediction of the possibility of delayed recovery is very important in terms of taking appropriate decisions on life-support withdrawal.
A study involving 104 unresponsive adults who had suffered a sudden brain injury caused by hemorrhage, trauma, or lack of oxygen, has found that about 15% of patients showed brain activities detected by EEG within 4 days of injury when they were subjected to motor commands, such as opening and closing of the hands.
This indicates the presence of hidden consciousness or cognitive capabilities. Of the patients with hidden consciousness, about 50% showed significant improvement and were capable of responding to the verbal instructions before hospital discharge.
After 1 year of injury, about 44% of patients with hidden consciousness were capable of performing normal daily activities without seeking any help. This indicates that patients with hidden consciousness are more likely to get eventual functional recovery than those who lack it.
Having higher functional integrity as well as better connections between the brain stem, thalamus, and cortex may be responsible for the hidden consciousness.
EEG-based detection of consciousness can also be used to distinguish between different types of consciousness disorders, such as persistent vegetative condition, minimally conscious condition, and coma. Although patients who are in a vegetative state do not show any sign of awareness, it has been found that about 40% of them possess minimal consciousness.
In this context, a study has shown that of 16 vegetative patients, three were capable of following and responding to verbal instructions similarly as their healthy counterparts. This indicates that EEG can be effectively used to accurately determine the consciousness state of a patient.
The benefits of using EEG over MRI are that EEG is less expensive, easy to perform, and can be used relatively easily in a critical care setup. However, certain points need to be taken into consideration while using EEG for detecting hidden consciousness.
Firstly, a patient should undergo EEG testing at least once or twice daily, because consciousness can fluctuate after a brain injury. Secondly, a high synchronization level should be maintained between the spoken commands and EEG recordings. Lastly, EEG monitoring should be initiated as early as possible after the injury to accurately predict hidden consciousness.
Last Updated: Jul 18, 2023