Gastritis refers to a group of disorders characterized by inflammation of the stomach lining. The inflammation is usually caused by infection with the bacteria that causes stomach ulcers – Helicobacter pylori (H. pylori). Other factors known to contribute to gastritis include injury, excess alcohol intake and the use of certain pain killers.
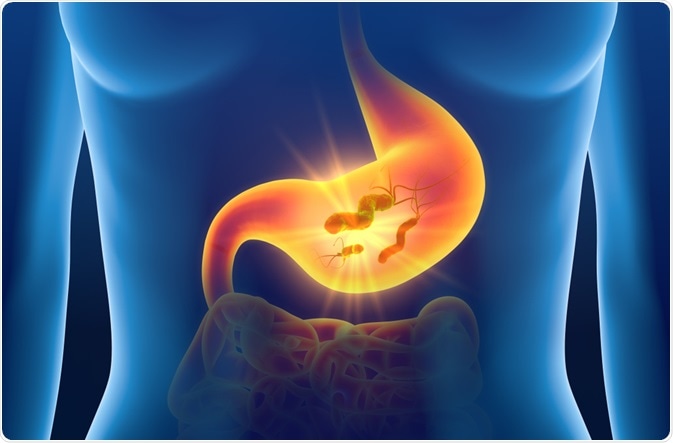 Image Credit: Axel_Kock/Shutterstock.com
Image Credit: Axel_Kock/Shutterstock.com
The signs and symptoms associated with gastritis include nausea, vomiting, gnawing pain in the upper abdomen and a feeling of fullness in the upper abdomen after food has been eaten.
If left untreated, gastritis can eventually cause stomach ulcers to develop and bleeding in the stomach. In rare cases, the illness can increase the risk of stomach cancer, particularly if the condition has caused extensive thinning of the lining in the stomach and changes to its cells. Diagnosing gastritis is therefore important so that treatment can be arranged and the condition managed as soon as possible.
Gastritis can be diagnosed based on a physical examination and the patient’s account of their symptoms. However, certain tests may also be required to help establish the exact cause of the condition. A step-by-step approach to diagnosing this condition is given below.
Patient history and physical exam
A doctor obtains a full medical history that should cover the use of any non-steroidal anti-inflammatory drugs (NSAIDs) or alcohol intake. Of people who use NSAIDs, up to 20% report indigestion symptoms. Gastrointestinal (GI) Symptoms related to the use of NSAIDs are more likely in patients who have had a previous GI event such as a hemorrhage or ulcer; those on a high dose of NSAIDs; those aged older than 60 years and those who also take corticosteroids or anticoagulants.
Any history of previous gastrointestinal surgery is also obtained along with the details of any autoimmune conditions that increase the risk of gastritis such as type 1 diabetes and hypoparathyroidism.
Investigations
- A gastroscopy may be performed, which is a type of upper gastrointestinal endoscopy. The procedure involves an endoscope being inserted into the patient’s stomach to examine the internal walls of the esophagus and stomach. This procedure is often used to confirm a diagnosis. If metaplasia (pre-cancerous changes) or gastric cancer is suspected, a biopsy sample may also be taken from the affected area.
- Blood tests may be carried out to check blood cell counts and the function of the liver, kidneys, gall bladder and pancreas.
- Tests for H. pylori are carried out. For those aged under 55 in whom there are no indicators of GI malignancy, H. pylori testing followed by the appropriate treatment is advised. Two highly specific and sensitive tests for this include the urea breath test and the fecal antigen test, which both detect active infection. These tests are also used to monitor patients after they have received treatment. The urea breath test is 96% specific and more than 90% sensitive in the detection of H. pylori. The fecal antigen test, which detects H. pylori in stool samples, is available as a monoclonal and polyclonal assay. The sensitivity and specificity of the monoclonal assay are 96% and 97%, respectively and for the polyclonal assay, both sensitivity and specificity are more than 90%.
- Mucosal biopsy samples can also be used to check for H. pylori. The sample is placed on a reaction strip or agar gel that contains urea, a pH indicator and a buffer. If H. pylori is present, the urea is converted to ammonia and bicarbonate, which is picked up as a change in color. The sensitivity and specificity of this test are 90% and 100%, respectively, providing the patient is not taking a proton pump inhibitor or antibiotic. The test is also not reliable in individuals with an acute GI bleed.
The surprising cause of stomach ulcers - Rusha Modi
Gastritis associated with alcohol or NSAID use
If initial testing indicates an absence of H. pylori, and the use of NSAIDs or alcohol is suspected as a cause of the gastritis, the patient is taken off NSAIDs or told to stop drinking and therapy is prescribed to relieve symptoms. If the patient is unresponsive to treatment, gastroscopy may be considered to try and establish the cause.
Autoimmune gastritis
In cases where gastritis related to an autoimmune condition is suspected, tests to assess the serum vitamin B12 and autoantibody level are arranged. If a patient has pernicious anemia, gastroscopy is advised to check for any gastric cancer. A full blood count may be performed to check for anemia.
Phlegmonous gastritis
Phlegmonous gastritis which occurs as the result of peptic ulcer, systemic infection, surgery, cancer, or other serious stress can be confirmed by performing a plain upper GI series or computed tomography. Nasogastric drainage should also be carried out to obtain gastric contents for culturing.
References
Further Reading
Last Updated: Jun 15, 2023