Glomeruli are at the heart of renal function, and yet are only part of an intact nephron. They are of irreplaceable value in maintaining homeostasis.
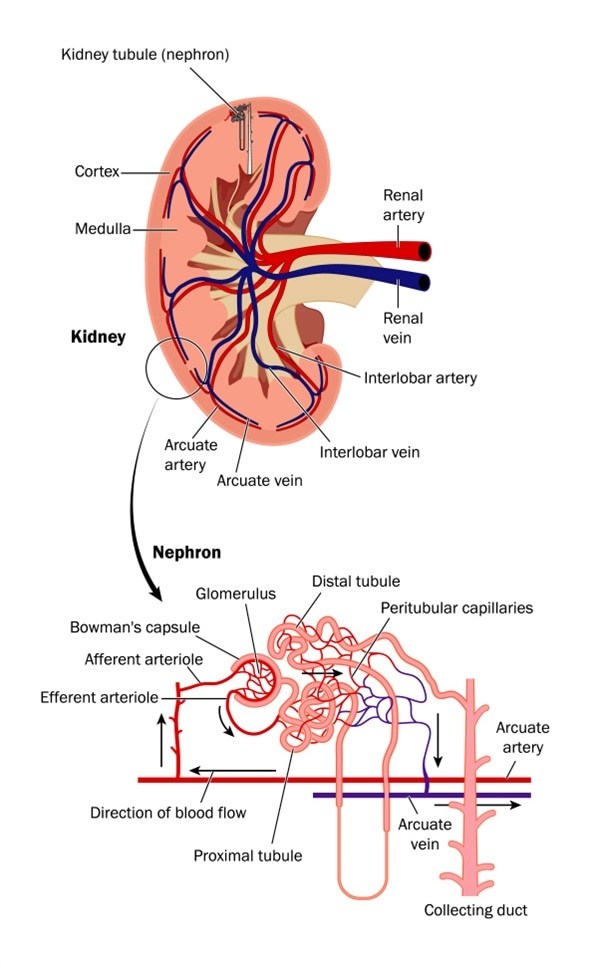
Cross section of kidney and diagram of nephron - Image Copyright: Blamb / Shutterstock
Functions of the glomerulus
Their functions may be briefly described as:
- Ultrafiltration of plasma which includes the removal of plasma solutes along with the water, at a rate of approximately 150 L/day
- Keeping the blood pressure normal by means of various hormonal and physical signals, mediated by the renin-angiotensin-aldosterone axis, which regulates the water-electrolyte balance of the body that is essential for life and normal functioning
- Regulating the blood flow through the peritubular network of arterioles, which directly affects tubular metabolism and kidney health
- Removing toxic macromolecular aggregates and complexes such as antigen-antibody complexes
Pathophysiology of glomerular injury
The pathophysiologic mechanisms of glomerular injury have been explained using three models:
- The intact nephron theory: Each nephron is a miniature kidney, and damage to one of the components causes injury to the entire nephron. This may be via defects of the peritubular capillary network, alterations in the composition of the urinary fluid passing down the tubule, reduction in the oxygen supply, and consequent metabolic deficits.
The consequences of nephron damage include lowered protein resorption by the nephron and reduced synthesis of important hormones such as 1,25-dihydroxy cholecalciferol and erythropoietin.
The outcome includes necrosis of the tubular epithelium, and failure of glomerular filtration because of the tubuloglomerular feedback. The eventual result may be one of several possibilities such as:
- Nephron repair
- Nephron loss due to irreversible damage
- Hypertrophy and hyperfunction of remaining healthy nephrons to compensate for nephron loss
- Fibrosis of damaged regions of the kidney, with consequent vascular insufficiency of the remaining nephrons, and progressive damage to the kidney
- The hyperfiltration theory: Another mechanism that has been observed to operate in rodent models is the damage caused by hyperfiltration across the glomeruli, as a result of higher hydrostatic pressure in the glomerulus. This was the effect of many drugs and chemicals which were toxic to the kidneys.
- The complex deposition theory: The finding that macromolecules in the circulation were primarily removed in the kidney was important in understanding this class of renal damage. Among the more important of these are soluble immune complexes. These are different from the normal antibody-antigen combinations, in that they have an excess of either antigens or antibodies and cannot precipitate from the circulation. These are then filtered out by the kidney, and deposit in various locations depending on their physical and chemical characteristics. Some deposit in the basement membrane under the endothelial cells, while others are found in the mesangium. The consequences may include inflammatory reactions, with or without complement activation. The end-result may often be glomerular destruction. Others may activate mesangial cells or induce secretion of excessive membranous proteins. These events may lead to permanent sclerosis of glomeruli. The whole kidney may be further damaged by hyperfiltration changes as well as alterations in the microcirculation of intact nephrons.
Mechanisms of glomerular injury
Drugs may induce glomerular injury via various mechanisms:
- Direct damage to the glomerular epithelium, as with Adriamycin
- Renal perfusion defects leading to glomerular injury, as with cyclosporine A
- Immunologic reactions such as immune complex formation, with gold and D-penicillamine
- Formation of anti-glomerular basement membrane antibodies, as in organic solvents
Thus there is a complex cycle of glomerular injury, loss of function of the nephron, stress to other nephrons, decreased perfusion as a result of fibrosis, leading to an extension of the injury, as well as hyperfiltration in remaining nephrons, which may result in progressive renal damage.
Classification
Glomerular injury may cause kidney disease of various types:
- Autoimmune disease: Systemic lupus erythematosus, IgA nephropathy, Goodpasture’s syndrome
- Post-infectious disease: Acute post-streptococcal glomerulonephritis, bacterial endocarditis
- Sclerotic disease: Glomerulosclerosis, diabetic nephropathy, focal segmental glomerulosclerosis
- Others: Membranous nephropathy, minimal change disease
References
Further Reading
Last Updated: Mar 16, 2023