The initial outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, was in Wuhan, Hubei province, China, in December 2019. As of March 2020, the virus has reached 120 million cases and caused over 2.66 million deaths worldwide.
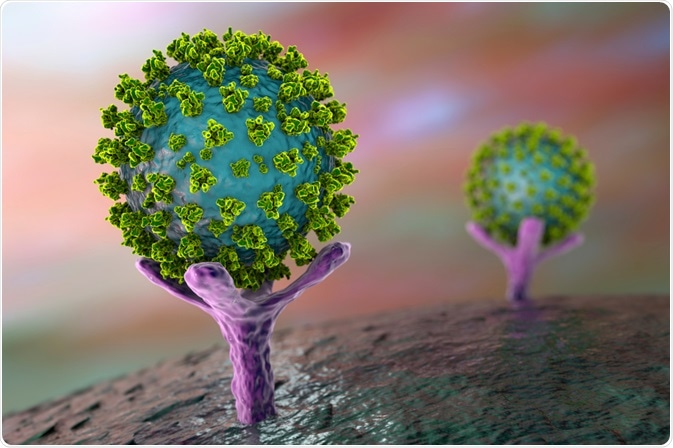 Image Credit: Kateryna Kon/Shutterstock.com
Image Credit: Kateryna Kon/Shutterstock.com
Comparing pandemics
There have been many comparisons made between the COVID-19 pandemic and previous pandemics, from the 2002 SARS and 2012 MERS pandemics to the 14th-century bubonic plague.
It can be difficult to make direct comparisons between pandemics as they all develop within specific circumstances, from the differing nature of the disease itself to the variable social and political contexts in which the pandemic develops.
For instance, the 1918 H1N1 influenza pandemic (commonly called Spanish Flu) occurred during World War 1, meaning that soldiers were traveling and spreading the virus around the world. With SARS-CoV-2, strict lockdown measures were put in place early in the pandemic, which limited the spread of the disease even within cities.
Additionally, scientific and medical advancements and knowledge of previous pandemics now help to understand, control, and stop pandemics. For instance, scientists are now able to identify novel diseases more easily, and containing outbreaks can be achieved more quickly as a result.
Hygiene practices are also much better in contemporary medical facilities as there is a greater understanding of how diseases spread. However, depending on how infectious the disease is and how severe the symptoms are, it is not guaranteed that epidemics, pandemics, or deaths can be avoided entirely.
The time it takes for a safe and effective vaccine can also extend the duration of a pandemic.
Disease origins
Diseases can spread to humans from many different sources, from bacteria spread through flea bites to viruses that jump from animals to humans.
The sources for seven major pandemics include:
- 1918 and 2009 influenza (H1N1): zoonotic influenza virus from pigs in 1918 and 2009.
- Avian influenza A (H5N1 and H7N9): zoonotic influenza virus from birds and poultry
- Bubonic plague: Yersinia pestis, a zoonotic bacteria found in fleas and small mammals
- COVID-19: a zoonotic coronavirus of unconfirmed origin as of March 2020. Most researchers believe it stemmed from a bat source with possible intermediate species (perhaps pangolins).
- Ebola: zoonotic Ebola virus from a bat
- MERS-CoV: zoonotic coronavirus possibly originally from a bat, transmitted to humans via dromedary camels
- SARS-CoV: zoonotic coronavirus from a bat
Disease spread
If an outbreak begins in a city, it typically spreads very quickly due to the close proximity of residents. This was seen in the SARS pandemic in Hong Kong in 2003, and with the Ebola pandemic in Conakry, Freetown, and Monrovia from 2014 to 2016.
SARS-CoV-2 spread very quickly from Wuhan throughout China in part because Wuhan is one of the most important traffic hubs in Central China. The outbreak of SARS-CoV-2 also came during the Spring Festival, meaning that large amounts of people were traveling in and out of Hubei province’s capital city Wuhan and spreading the virus throughout the country.
Increased globalization, which has seen increasingly large amounts of people regularly traveling globally, has also allowed the SARS-CoV-2 virus to spread quickly throughout countries, and it has only taken a matter of months to reach almost every country in the world.
However, unlike SARS-CoV-2, not all viruses are spread through droplets in sneezes and coughs.
The different disease transmissions for seven major pandemics include:
- 1918 and 2009 influenza (H1N1): respiratory droplets, infected surfaces
- Avian influenza A (H5N1 and H7N9): H5N1 is spread by contact with infected living or dead poultry and birds or rarely prolonged contact with infected humans; H7N9 is spread through contact with infected poultry.
- Bubonic plague: flea bites
- COVID-19: respiratory droplets, unconfirmed: feces, other bodily secretions (the virus can be present in these secretions, but it is unconfirmed whether it is infectious).
- Ebola: contact with infected blood or body fluids
- MERS-CoV: respiratory droplets
- SARS-CoV: respiratory droplets

Image Credit: Jarun Ontakrai/Shutterstock.com
Case and fatality rates
A case fatality rate (CFR) shows the number of reported deaths per number of reported cases. These numbers can vary significantly depending on a population’s ability to report cases or deaths to health organizations tracking pandemic statistics.
In the case of COVID-19, a high number of people can be asymptomatic and unaware that they have been infected with the disease. This means that they are unlikely to get tested and report a confirmed case of COVID-19 to health organizations, which can lead to case rates being higher than the statistics show.
The global case rates and case fatality rates for six major pandemics are:
- 1918 influenza (H1N1): 50 million; CFR 2%-3%.
- Avian influenza A (H5N1 and H7N9): H5N1 had 649 cases; 60% CFR; H7N9 had 571 cases; 37% CFR.
- COVID-19: ~2.1 (variable estimates due to ongoing pandemic)
- Ebola: over 30,000 cases; average 50% CFR.
- MERS-CoV: 2,502 cases; 34% CFR.
- SARS-CoV: 8,422 cases; 15% CFR.
The bubonic plague during 1347 and 1351 saw extremely high numbers of deaths, largely due to poor hygiene, a lack of understanding around disease spread, and large numbers of people living in very close proximity to each other.
Although specific case rates are not available, 30 to 50 percent of the European population died from the plague. Now, it can be successfully treated with antibiotics, although there are still between 1,000 to 2,000 cases reported to the World Health Organization worldwide every year.
Summary
History has seen many pandemics emerge and conclude, with medical and scientific understanding, living conditions, and socio-political contexts all playing a part in how the pandemic is identified, controlled, and stopped.
The diseases themselves also differentiate pandemics from each other, as some viruses or bacterial infections cause more severe symptoms and affect different populations, who may be more vulnerable than others. For instance, COVID-19 mainly causes severe symptoms in people over 65 and those with underlying health conditions, whereas the 1918 influenza caused severe symptoms in young and healthy populations.
Reporting confirmed cases accurately and providing accessible testing are particularly helpful methods in understanding an evolving pandemic like COVID-19, as this allows health organizations and governments to control the spread of the virus within their environments and offer effective advice to help people stop the spread and protect themselves against infection.
References
Further Reading
Last Updated: Mar 16, 2021