Corneal inflammation or keratitis is caused by germs such as bacteria, viruses, parasites, and fungi. Physicians employ both traditional and new techniques to diagnose keratitis. However, the success rate depends on the accurate diagnosis, expertise of the physician and microbiologist, and the availability of facilities.
Diagnosis symptoms
Viral keratitis is caused by the virus Herpes Simplex Virus (HSV). HSV-1 (one category of HSV) infections show symptoms such as cold sores in the mouth, which is the most common site of infection. When other parts of the body are infected, the infection is reactivated. The virus is present only in humans and can spread by direct contact with an infected person. In the case of viral keratitis, the history of the patient is examined and diagnosis is based on the eye examination.
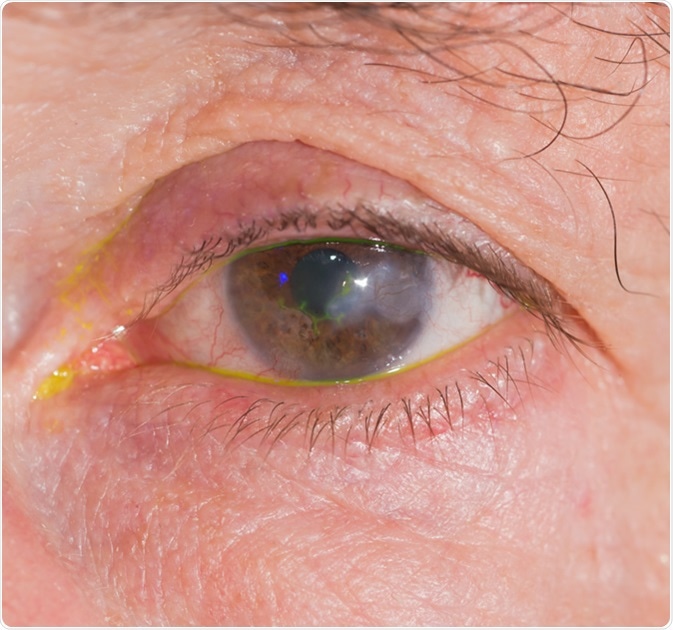
Close up of eye examination, Herpes keratitis. Image Credit: ARZTSAMUI/Shutterstock
Symptoms such as pain in the eye, red eye, blurred vision, photophobia, discharge/excessive tearing from the eye are common for all types of keratitis. In addition to these general symptoms, patients of Acanthamoeba keratitis may experience a sensation of foreign particles in the eye.
Depending on the diagnosis required, physicians decide on the type of samples to be collected.
Sample types
Corneal scraping is collected using a Kimura spatula, a No.15 surgical blade, or a bent needle. Lamellar biopsy techniques are used in corneal biopsy samples when the infection is deep-seated. In keratitis of non-healing types, penetrating keratoplasty is done in corneal buttons. Samples such as contact lenses, lens solution, and lens cases are tested when physicians suspect contact lenses to be the causing agent of the keratitis.
The collected samples are tested using a variety of stain methods for smears. In many cases, initial smear tests provide a faster diagnosis. Smears are not made from samples such as corneal biopsy, corneal buttons, contact lens, lens solution, and lens cases. These samples are sent to the laboratory to be processed directly for detecting the culture of fungi, bacteria, or parasites.
Smear tests
Gram stain is the most widely used stain. Acridine orange stains help in detecting the presence of most microorganisms. Organisms such as fungi, bacteria, and microsporidia or acanthamoeba parasites can be detected using staining methods such as Lactophenol cotton blue, KOH with Calcofluor white, and Gomori methenamine silver stains.
The presence of Actinomycetales is shown by the Gram-positive, beaded, thin, branching filaments in the sample. When using modified Ziehl Neelsen stain with 1% of H2SO4 (Kinyoun stain), the presence of acid-fast filaments in the sample reveals Nocardia infections.
Laboratory testing is not usually carried out for viral keratitis, except to confirm the presence of viruses such as HSV-1. Nonspecified staining methods such as Papanicolaou, Giemsa, and Hematoxylin-eosin stains are used for the rapid detection of viral infection. In particular, Giemsa stains are ideal for cell-type evaluation and are found to be useful to detect viral keratitis.
Indirect immunoperoxidase (IP) assays and immunofluorescence (IF) — both direct and indirect categories —are used in the diagnosis of viral pathogens. The advantage in using indirect immunoperoxidase (IP) lies in its ability to be used on paraffin-embedded tissue. Indirect immunofluorescence (IF) assay is found to give better outcomes when using frozen tissue samples.
Culture methods
While primary results of the samples are obtained using the smear method, confirmation of the disease is done by carrying out culture isolation. For corneal scraping samples, thioglycollate broth culture is carried out to confirm the bacterial presence.
While Sheep blood agar is used as the culture medium to detect bacteria and fungi in intraocular lens/iris tissue samples, aerobic and anaerobic sheep blood agar, non-nutrient agar with E.coli and Sabouraud dextrose agar are used for samples such as contact lenses and contact lens solutions.
In addition, sheep blood chocolate agar and brain–heart infusion broth are also employed in corneal scraping, corneal biopsy, and corneal button samples to confirm the presence of bacterial, fungus, or acanthamoeba keratitis.
Prior knowledge about the suspected organism helps to select the right type of culture media. Depending on the media, the incubation conditions vary. The process to isolate bacteria and fungi is carried out in most samples. Pseudomonas aeruginosa and Staphylococcus aureus are the two common bacteria that cause bacterial keratitis.
The species Fusarium, Aspergillus, and Candida are said to cause fungal keratitis. Fungi related to eye infection grow faster, while slower growth is seen in atypical mycobacteria and Nocardia bacteria species and the Acanthamoeba parasite.
Staphylococcus aureus (Illustration): Image Credit: Tatiana Shepeleva / Shutterstock
Confocal microscopy is a non-invasive method that helps to visualize the cornea. It helps in repeated observations and supports the diagnosis of even hazy corneas. In cases where profound corneal infiltrate are noticed, confocal microscopy is used for diagnosis. A close-up examination of the eye using confocal microscopy will allow the physician to view the amoeba, the single-celled living organism that causes Acanthamoeba keratitis.
Molecular techniques such as polymerase chain reaction are used to diagnose viruses or to find organisms that take more time to grow or that are complex for the culture method.
Keratitis - Bacterial and Fungal
References
Further Reading
Last Updated: Jul 24, 2023